Understanding Morton’s neuroma
You may notice a small “lump” or bunched‑up feeling between the toes—most often between the third and fourth toes (third webspace). Typical signs include a burning or stabbing pain in the ball of the foot, sharp shooting pain into the adjacent toes, tingling or numbness, and the sensation of walking on a pebble. Symptoms often worsen in close or high‑heeled footwear and settle when pressure is reduced.
What it is
Although it can feel like a lump, it isn’t a tumour. Morton’s neuroma is a benign thickening of tissue (perineural fibrosis) around a small forefoot nerve (the common digital nerve). It’s your body’s response to repeated compression and irritation. As the tissue thickens, the space between the metatarsal heads (the ball of the foot) narrows further, which increases pressure on the nerve—hence the pain.
Why it develops—and why the pain can be sharp or shooting
The rounded ends of the long bones in your forefoot (metatarsal heads) sit side by side, with the common digital nerve running between them—most often between the third and fourth toes. As your weight rolls forward—especially in narrow toe boxes or higher heels—those bones press on the nerve. Repeated pinching irritates the nerve and nearby tissues, which produces burning, tingling, and sharp, shooting pain into the toes. Long hours on firm surfaces and forefoot‑heavy activities magnify the irritation.
Quick self‑check (not a diagnosis)
If this description sounds familiar, the simple checks below can help you judge whether the nerve between the metatarsal heads is likely involved. Go gently and stop if pain is sharp.
Step 1 — Where it hurts: neuroma pain is typically felt between the third and fourth toes and can shoot into those toes (common plantar digital nerve in the third webspace). Pain directly under the big toe or at the base of the second toe usually points to a different problem.
Step 2 — Gentle forefoot squeeze: place one hand on each side of the forefoot and gently squeeze side‑to‑side. If this brings on a sharp, electric‑type pain into the toes or a small click/snapping sensation, it suggests irritation of the interdigital nerve between the metatarsal heads.
Step 3 — Try different shoes: compare a narrower or higher‑heeled pair with a roomier, flatter pair. If pain is worse when the toe box is tight or the heel is raised—and easier when the forefoot can spread—crowding and forefoot load are likely aggravating the nerve.
Step 4 — Toe‑spacing check: standing, gently spread the toes or try a slim, soft spacer between the affected toes (only if comfortable). If this eases the “pebble”/burning sensation, a little extra space between the metatarsal heads is helping to reduce nerve pressure.
What to do next
If two or more of the checks suggest Morton’s neuroma, your next step is to reduce pressure between the metatarsal heads and soften forefoot impact with the right insole set‑up. If your symptoms don’t match—or you’re unsure—see the list of other common causes below and consider a professional assessment.
Other common causes of forefoot pain (how they differ from Morton’s neuroma)
Not all ball‑of‑foot pain is a neuroma. These are frequent culprits and the key differences to look for:
- Second‑toe capsulitis / plantar plate strain — irritation or small tears at the base of the second toe (second MTP). Differs from a neuroma by pinpoint pain right on the joint line and pain when the second toe is bent upwards; the toe may feel “unstable” or drift toward the big toe; usually no shooting, electric pain into two toes.
- Metatarsal stress injury (reaction or fracture) — overuse bone stress, most often in the second or third metatarsal. Differs by a very focal “one‑spot” bony tenderness that hurts with hopping and may ache at night; tingling into the toes is uncommon.
- Sesamoiditis (under the big‑toe joint) — irritation of the two small sesamoid bones beneath the first MTP. Differs by sharp, localized pain directly under the big toe at push‑off, rather than a “pebble” feeling between two toes or shooting into adjacent toes.
- Tarsal tunnel irritation — compression of the posterior tibial nerve near the inner ankle. Differs by tingling/burning that starts at the inner ankle and radiates more broadly into the sole, not limited to a single webspace.
- Interdigital bursitis — inflammation of a small fluid‑filled sac between metatarsal heads. Can mimic a neuroma but usually feels like aching or a sense of fullness in the webspace with tender swelling; less likely to cause electric, shooting pain.
- MTP joint synovitis or osteoarthritis — inflammation or wear affecting one or more toe joints. Differs by joint‑line tenderness, morning stiffness, and pain when the toe bends, rather than squeeze‑provoked pain between two toes.
- Forefoot fat‑pad thinning (atrophy) — loss of the natural cushioning under the metatarsal heads. Differs by a broad, bruise‑like soreness across the ball of the foot on firm floors, without electric pain into adjacent toes.
- Gout at the big‑toe joint — sudden, very painful, hot, red swelling of the first MTP. Differs by acute inflammatory signs at one joint (often at night) rather than a “pebble” between two toes with electric‑type pain.
- Peripheral neuropathy — nerve irritation or damage causing burning, tingling, or numbness, often in both feet. Differs by a diffuse, symmetrical “stocking” pattern instead of one specific webspace with squeeze‑provoked pain.
- Morton’s toe / metatarsal parabola variation — a relatively long second metatarsal shifts pressure centrally. Not a neuroma by itself, but it can create central hotspots and, over time, irritate nearby nerves; pain is primarily load‑driven rather than electric.
- Hammer or claw toes — bent toes creating pressure on the knuckles and under matching metatarsal heads. Differs by corns/callus on the toe knuckles and pinpoint pressure pain under specific heads rather than between‑toe shooting pain.
If you want confirmation
Building on your self‑check, a clinician will perform the Mulder test during a structured foot exam: beyond the gentle squeeze, they add focused pressure in the suspected web space, may lift the toes slightly, and compare with the neighbouring spaces to see whether it exactly reproduces your pain or a small ‘click’. They’ll also assess toe alignment, bunions, and support across the forefoot (transverse arch) and—when appropriate—use a small local anaesthetic injection to confirm the source. Ultrasound imaging can help confirm the diagnosis by showing a thickened interdigital nerve consistent with a neuroma and by ruling out other causes.
Reduce day‑to‑day irritation
Whether you’re waiting for an appointment or managing it on your own, start by easing what squeezes or irritates the nerve day to day. Then add targeted support to create space and share pressure so walking feels natural again.
Factors that increase the squeeze
A few common factors ramp up pressure between the metatarsal heads. Look for these and change what you can.
- Footwear: narrow toe boxes crowd the toes; higher heels shift more load to the forefoot.
- Prolonged standing or firm floors: increase peak pressure beneath the metatarsal heads.
- Foot mechanics: limited ankle bend (reduced dorsiflexion), a dropped forefoot arch (transverse arch), bunions (hallux valgus), flat feet (pes planus), and high arches (pes cavus) can focus load in one nerve space.
- Activities that load the forefoot: running, brisk hill walking, court and field sports, rope work, jumping drills, forefoot‑dominant dance styles.
What you can do now (first‑line relief)
Make a few simple changes to lower forefoot pressure and settle irritation. Choose roomier shoes with a wider, rounder toe box and a moderate heel; set very high heels aside for now. Pace your activity by trimming high‑impact or hill sessions and taking brief breaks during long periods of standing. Wear softer, seamless socks and adjust lacing so the forefoot has a little give while the heel stays secure. Add a short daily routine—calf stretches, gentle big‑toe extension, and light foot‑intrinsic work (towel scrunches)—to support the transverse arch. During flares, a slim toe spacer can reduce rubbing if it feels comfortable in your shoes.
Why acting early helps
When pain hangs around, you naturally shorten steps, lift the heel early, or tip weight to one side to dodge the sore spot. Over time, those habits can shift strain to your ankle, knee, hip, or lower back. Reducing nerve compression now helps you return to a more natural stride and prevents “chasing” pain elsewhere.
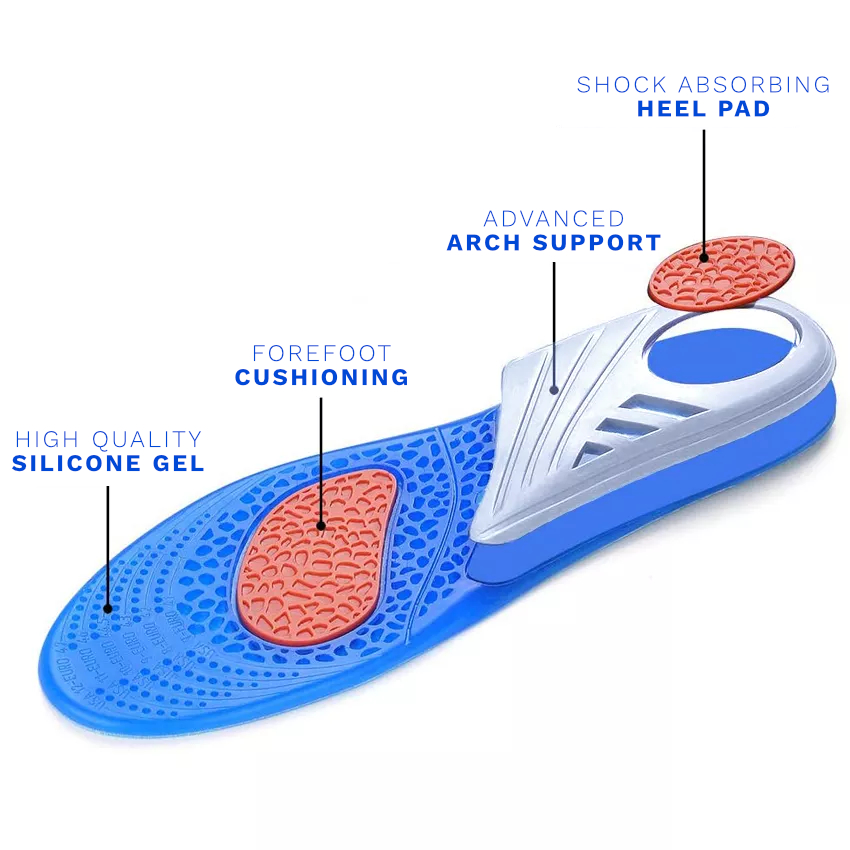
Why orthotic insoles are a smart first step
After you ease the day‑to‑day squeezes, orthotic insoles give you targeted support that reduces pressure on the nerve with every step. Position the metatarsal support just behind the ball of your foot (proximal to the metatarsal heads); this gently spreads the metatarsals, increases space around the interdigital nerve, and takes the sting out of push‑off. Forefoot cushioning then lowers the jolt and rubbing that keep the area irritated, while the overall contour guides a steadier roll‑through so you stop guarding the sore spot. There’s solid clinical evidence for this approach: neuroma reviews and broader foot‑pain research show that metatarsal support and well‑designed orthoses can reduce forefoot pressure, ease pain, and improve function (Thomson et al., 2004; Neal et al., 2018; Landorf et al., 2006). In practice, you should feel a gentle “spread” rather than a poke under the forefoot, a softer feel as you push off, and a more natural, easier stride as irritation settles.
Fit and break‑in: what to expect
Place the insole flat in your shoe and slide your foot back so your heel rests comfortably in the heel cup. Check that the highest part of the metatarsal support sits just behind—not on—the sore spot; you’re aiming for subtle lift and space, not pressure. Gradually increase wear time over 1–2 weeks: start with an hour or two for the first couple of days, move toward half‑days, and aim for most of the day in week two. It’s normal to notice a “new support” feel that fades within minutes; the ball‑of‑foot burn should feel calmer, not sharper. Pair the insoles with a wider, rounder toe box and a moderate heel height so your forefoot can spread and the insole can do its job. If you feel direct pressure on the sore spot, adjust the insole slightly back until the support sits behind it; if numbness increases, ease back wear time for a day and then rebuild.
If symptoms persist: injections and surgery at a glance
Most people improve with the changes above and well‑fitted insoles. If sharp, shooting pain is still limiting you after 4–6 weeks of consistent use, arrange a review. Your clinician can advise on next‑step options such as image‑guided corticosteroid injections; a procedure on the thickened nerve is usually considered only when conservative care hasn’t helped enough (Sharp et al., 2003; Dockery, 1999). You can talk through likely benefits, risks, and recovery time for each option and decide together what suits you best.
Ready to get started?
Fit FootReviver Morton’s Neuroma Insoles into your shoes. Make sure the metatarsal support sits just behind—not on—the sore spot, and gradually increase wear time over 1–2 weeks. Pair with roomier footwear and the simple daily routine above for the best results.
References for this section
- Thomson, C. E., Gibson, J. N. A., & Martin, D. (2004). Interventions for the treatment of Morton’s neuroma. Cochrane Database of Systematic Reviews, (3), CD003118.
- Neal, B. S., Nester, C., Uden, H., & Searle, A. (2018). The effectiveness of footwear and orthotic devices in the management of foot pain and function in adults: A systematic review. Foot & Ankle Surgery, 24(3), 185–191.
- Landorf, K. B., Keenan, A. M., & Herbert, R. D. (2006). Effectiveness of foot orthoses to treat plantar fasciitis: a randomised trial. Archives of Internal Medicine, 166(12), 1305–1310.
- Sharp, R. J., Wade, C. M., Hennessy, M. S., & Saxby, T. S. (2003). The role of MRI and ultrasound imaging in Morton’s neuroma. Journal of Bone and Joint Surgery (Br), 85‑B(7), 999–1005.
- Dockery, G. L. (1999). The treatment of intermetatarsal neuromas with 4% sclerosing alcohol injection. Journal of Foot & Ankle Surgery, 38(6), 403–408.
Other conditions these insoles can help with
For Overpronation
Overpronation: what it is, why it happens, and how it links to forefoot pain (including Morton’s neuroma)
In a normal step, your foot rolls in a little (pronates) to absorb shock and then rolls out to push off. With overpronation, the inward roll goes too far or lasts too long. The inner arch (medial longitudinal arch) flattens, the heel tilts in (rearfoot eversion), and the shin turns inward. This raises strain on the posterior tibial tendon and plantar fascia and shifts pressure toward the centre of the forefoot—often under the second and third metatarsal heads. As the transverse arch at the ball of the foot flattens, the metatarsal heads press closer together, narrowing the space for the interdigital nerve. That squeeze can irritate the nerve and contribute to Morton’s neuroma.
Who’s most at risk and why
- Flexible or low arches; family tendency to “roll in”; hypermobility
- Pregnancy, higher body weight, or long days on firm surfaces
- Sudden increases in walking or running without gradual progression
- Thin, worn, or very soft shoes that let the heel tip in and the arch collapse
Where it hurts and what to look for
- Ache along the inner arch or just behind/above the inner ankle (posterior tibial tendon)
- Burning or hard skin under the second/third metatarsal heads; “hot pebble” sensation
- Shin ache or inner‑knee discomfort after longer walks or hills; shoes worn on the inner edge
First steps that help
- Footwear: supportive midsole, firm heel counter, wider base; replace very worn soles
- Strength/mobility: short‑foot drills, towel scrunches, calf stretches, and hip/glute work
- Pacing: build distance and hills gradually; add softer‑surface sessions during flares
How FootReviver orthotic insoles help overpronation and neuroma‑type forefoot pain
- Support the arch under load: a defined arch contour limits collapse in mid‑stance, easing strain on the posterior tibial tendon and plantar fascia and reducing inward rotation that drives pressure into the central forefoot.
- Improve heel landing: a cupped, reinforced heel cradle helps you land more upright so the step starts stable, not rolled‑in.
- Create space and share pressure at the ball of the foot: increased midfoot contact and a correctly positioned metatarsal support (just behind the metatarsal heads) gently spread those bones, easing pressure on the interdigital nerve and reducing high‑pressure points under the second/third heads.
Take a practical step. Fit FootReviver Morton’s Neuroma Insoles (trim the forefoot to size), ensure the arch feels supportive (not intrusive), set the metatarsal support just behind—not on—the sore spot, and increase wear time gradually.
For Supination
Supination (underpronation): what it is, who it affects, and how it links to forefoot irritation
Normally, the foot rolls in slightly to absorb shock. With supination (underpronation), the foot stays rolled outward on the ground. It often pairs with a higher, stiffer arch, so less of the sole contacts the ground and shock absorption is reduced. Load concentrates on the outer border of the forefoot (fourth/fifth metatarsal heads) and ankles can feel less stable. When push‑off is biased to the outside, the metatarsal heads do not spread evenly and the central spaces can still be squeezed with each step—one way a Morton’s neuroma can be irritated even in a “high‑arch/supinated” foot.
Who’s most at risk and why
- Higher, rigid arches or a history of ankle “rolls” on uneven ground
- Tight calves and reduced ankle mobility (less natural shock absorption)
- Minimal or very worn shoes that lack cushioning and side‑to‑side control
- Sudden increases in pace, downhill sessions, or cambered routes
Where it hurts and what to look for
- Ache along the outer foot; hard skin under the fourth/fifth metatarsal heads
- Recurrent ankle sprains or a “tippy” feeling on cambers or gravel
- A jarring feel on firm ground; soreness after faster work or long shifts
First steps that help
- Footwear: cushioned, supportive shoes with secure heel counters and good midfoot structure
- Strength/mobility: balance training, peroneal (outer calf) strengthening, gentle calf stretches
- Pacing: build distance and pace gradually; vary surfaces to include some softer ground
How FootReviver orthotic insoles help supination and neuroma‑type forefoot pain
- Increase contact area (without forcing the arch flat): a contoured arch brings the midfoot into play so more of the sole shares load, reducing concentrated pressure at the outer forefoot and easing shear across the central spaces.
- Stabilise landing: a cupped heel resists outward tilt at heel strike so the ankle feels more secure and landing is more controlled.
- Balance push‑off and protect the nerve: subtle support just behind the ball of the foot and forefoot cushioning spread pressure across all metatarsal heads, helping prevent focal squeezing of the interdigital nerve.
Make a simple change. Fit FootReviver Morton’s Neuroma Insoles (trim to size), ensure the arch feels supportive and the heel well seated, position the metatarsal support just behind—not on—the sore area, and increase wear time gradually.
For Flat Feet
Flat feet (pes planus): what it is, who’s at risk, and why the ball of the foot often flares
In a normal step, the arch rises and falls slightly to absorb shock. With flat feet, the inner arch sits lower and often collapses further as you load the foot. The heel tilts in (rearfoot eversion), the midfoot unlocks, and the shin turns inward—raising work for the posterior tibial tendon and plantar fascia. At the front of the foot, the transverse arch flattens and the metatarsal heads press closer together, pushing more load beneath the central heads (second/third). That combination—more pressure and less space—can irritate the interdigital nerve, so ball‑of‑foot pain and Morton’s neuroma commonly appear alongside flat feet.
Who’s most at risk and why
- Flexible low arches or a family tendency to “roll in”; hypermobility
- Pregnancy, higher body weight, or long days on firm surfaces
- Prior ankle/foot injury; unsupportive, very worn, or soft shoes
Where it hurts and what to look for
- Ache along the inner arch or inside ankle (posterior tibial tendon area)
- Burning or hard skin under the second/third metatarsal heads; pebble‑like pain at push‑off
- Heel/arch soreness after longer walks; shoes wearing more on the inside
First steps that help
- Footwear: supportive shoes with a firm heel counter, stable midsole, and wider base
- Strength/mobility: short‑foot drills, towel scrunches, hip/glute work, and calf stretches
- Pacing: progress distance and hills gradually; add softer‑surface sessions during flares
How FootReviver orthotic insoles help flat feet and neuroma‑type forefoot pain
- Support the arch under load: a defined arch contour limits collapse in mid‑stance, easing strain on the posterior tibial tendon and plantar fascia and reducing inward rotation that drives load into the central forefoot.
- Land more upright: a cupped heel helps the heel land straighter so each step starts stable with less inward tilt.
- Reduce central pressure and protect the nerve: increased midfoot contact spreads load, and a correctly placed metatarsal support (just behind the ball of the foot) gently opens space between the metatarsal heads to ease pressure on the interdigital nerve.
Make a simple, effective change. Fit FootReviver Morton’s Neuroma Insoles (trim‑to‑fit), check the arch feels supportive, set the metatarsal support behind—not on—the sore spot, and build wear time gradually.
For High Arches
High arches (pes cavus): why pressure concentrates—and how to spread it to protect the forefoot
With a typical arch, more of the sole contacts the ground as you load the foot, which helps absorb shock. In high arches, the midfoot stays higher and contacts the ground less, so the heel and the ball of the foot take more of the load. To gain grip, the toes may claw, which flattens the transverse arch and raises pressure under the metatarsal heads—often beneath the first and central heads. These concentrated pressure points and subtle toe changes can narrow the spaces between the metatarsal heads, irritate the interdigital nerve, and contribute to Morton’s neuroma in some people with cavus feet.
Who’s most at risk and why
- Rigid, higher arches from adolescence or following prior injury
- Reduced ankle mobility or very tight calves (less shock absorption)
- Minimal/worn footwear on firm surfaces; frequent downhill or speed work
- A history of frequent ankle “rolls” or forefoot hotspots
Where it hurts and what to look for
- Burning or aching under the ball of the foot (metatarsal heads); toe clawing or corns
- Hard skin beneath the first or fifth metatarsal heads
- A “hard” or jarring feel on firm surfaces; outer‑ankle insecurity
First steps that help
- Footwear: cushioned, supportive shoes with secure heel counters and a little forefoot flex; slightly rockered soles often help on longer walks
- Mobility/strength: gentle ankle/calf mobility, balance training, and peroneal (outer calf) strengthening
- Pacing: build volume gradually; mix softer‑surface sessions
How FootReviver orthotic insoles help high arches and neuroma‑type forefoot pain
- Increase contact area (without flattening the arch): a contoured shape brings the midfoot into play so pressure is shared across more of the sole instead of concentrating on small areas.
- Cushion where you feel it most: silicone‑gel forefoot and heel zones soften landings on firm ground, easing irritation at sensitive metatarsals or sesamoids and reducing rubbing over the nerve.
- Add rearfoot control and forefoot space: a cupped heel reduces side‑to‑side wobble at landing, and a subtle metatarsal support set just behind the ball of the foot gently spreads the metatarsal heads to protect the interdigital nerve.
Feel the difference on firm ground. Trim FootReviver Morton’s Neuroma Insoles to size, ensure the arch feels supported and the heel well seated, position the metatarsal support just behind—not on—the sore spot, and increase wear time gradually.
For Metatarsalgia
Metatarsalgia: what it is, why it flares, and how to offload it
In a normal step, load passes across the ball of the foot (metatarsal heads) and on to the toes. Metatarsalgia is when peak pressure focuses under one or more metatarsal heads and becomes painful. It often follows training or walking increases, long days on firm surfaces, thin or narrow footwear, age‑related fat‑pad thinning, or toe deformities (e.g., hammer toes) that push more force onto a single ray. A relatively long second metatarsal or a bunion that shifts push‑off away from the big toe can also contribute.
Who’s most at risk and why
- Runners and brisk walkers adding distance or pace too quickly
- Standing long hours on firm floors in thin‑soled or tight shoes
- Older adults (fat pad thins with age)
- Foot shapes with a long second metatarsal, bunion, or lesser toe deformities
Where it hurts and what to look for
- A sharp or aching “stone‑bruise” under one or two metatarsal heads
- Pain that worsens with standing, push‑off, and barefoot on firm surfaces
- Localised tenderness and hard skin (callus) over the same spot
- Burning or tingling into the toes if a nearby interdigital nerve is also irritated
Why treatment matters
If you keep loading the same focal point, pain persists, callus can crack, and you may change your stride—often creating new sore spots.
Treatment options (start here)
- Footwear: wider, rounder toe boxes with some forefoot cushioning and modest flex; slightly rockered soles often help on longer walks
- Training habits: build distance/pace gradually; add softer‑surface sessions; reduce hill work during flares
- Foot care/strength: gentle toe mobility, towel scrunches, short‑foot work, and calf stretches to improve roll‑through
- Padding: a simple pad behind the painful area in roomy shoes
- Insoles: orthotic insoles that offload the exact sore head(s), reduce shear, and soften impact
How orthotic insoles help metatarsalgia
- Offload the hotspot: a metatarsal support pad placed just behind the painful area (proximal to the metatarsal heads) shifts peak pressure slightly back and spreads load—directly reducing the focal sore point.
- Reduce shear and impact: a smooth, low‑friction top cover and silicone‑gel forefoot cushioning soften the feel of pavements and firm surfaces and reduce rubbing over tender skin.
- Improve late‑stance sharing: a supportive arch and cupped heel help you move from heel landing to push‑off more consistently, so you don’t keep dumping load onto the same metatarsal head.
Take a practical step. Fit FootReviver Morton’s Neuroma Insoles (trim the forefoot to size), ensure the metatarsal support sits just behind—not under—the sore spot, and increase wear gradually. If pain doesn’t improve, speak to a healthcare professional.
For Plantar Fasciitis
Plantar fasciitis: what it is, who’s at risk, and how to support recovery
The plantar fascia is a strong band under the foot that supports the arch from the heel bone (calcaneus) to the toes. In a normal step, it stretches slightly and tightens as the toes bend upwards (windlass action). With plantar fasciitis, the fascia is irritated where it joins the heel or along the arch. The hallmark is sharp heel pain with the first steps after rest, easing as you warm up but often returning after long standing or by day’s end.
Who’s most at risk and why
- Flat feet (more elongation/strain) or high arches (less shock absorption)
- Sudden increases in running, walking, or hill work; new standing‑all‑day roles
- Firm surfaces, thin or unsupportive soles, or very worn footwear
- Tight calves (reduced ankle dorsiflexion) increasing pull on the fascia
Where it hurts and what to look for
- Heel pain at the inner front of the heel bone (medial calcaneal area), sometimes radiating along the arch
- “First‑step” pain in the morning or after sitting
- Discomfort after longer standing or brisk walking on firm ground
- Soreness that eases with gentle movement but returns with overload
Why treatment matters
Persisting pain can change how you walk—often shifting pressure forwards—leading to new discomfort under the ball of the foot and slower recovery.
Treatment options (start here)
- Footwear: supportive shoes with a firm heel counter, cushioned heel, and some midfoot structure; replace very worn soles
- Mobility/loading: daily calf and plantar fascia stretches; progress walking/running gradually; reduce hills during a flare
- Short‑term support: simple taping or a soft heel cup in irritable phases (when advised)
- Insoles: orthotic insoles to cushion the heel, reduce fascia strain, and prevent compensatory forefoot overload
How orthotic insoles help plantar fasciitis
- Cushion and seat the heel: a cushioned, cupped heel reduces the jolt at landing (heel strike) and positions the heel consistently, lowering strain where the fascia starts.
- Support the arch under load: a defined arch contour shares load during mid‑stance so the fascia is less tensioned step‑to‑step, reducing end‑of‑day soreness.
- Prevent knock‑on forefoot overload: if you’ve shifted pressure forward to avoid heel pain, subtle forefoot support and silicone‑gel cushioning help keep push‑off pressure shared.
Start simply. Fit FootReviver Morton’s Neuroma Insoles (trim at the forefoot for an accurate fit), ensure the heel feels seated and the arch supported, and build wear time gradually. Pair with daily stretches. If pain persists or night pain develops, speak to a healthcare professional.
For Bunions
Bunions (hallux valgus): what it is, why it develops, and how to reduce pain
Normally, the big toe (hallux) stays reasonably straight and helps you push off through the first metatarsophalangeal joint (first MTP). A bunion forms when the big toe drifts towards the second toe and the first MTP becomes prominent on the inner edge of the foot. Two problems follow: the bunion area rubs in footwear, and push‑off through the big toe is less effective, so load “transfers” to the second and third metatarsal heads.
Who’s most at risk and why
- Family history, female sex, and ligament laxity (softer connective tissues)
- Narrow or tapered toe boxes and higher heels that crowd and angle the toes
- Foot shapes with a long first metatarsal or a mobile first ray (first metatarsal not supporting push‑off well)
- Inflammatory arthritis that irritates/destabilises the big‑toe joint
Where it hurts and what to look for
- A visible bump at the base of the big toe with redness, swelling, or rub marks in shoes
- Callus or pain under the second/third metatarsal heads (“transfer” metatarsalgia)
- Stiffness or aching around the first MTP after long walks or on firm surfaces
- Toes crowding or overlapping in tighter footwear
Why treatment matters
Ignoring bunion pain can lead to stubborn skin problems, progressive deformity, and reduced walking tolerance. Early changes often reduce symptoms markedly.
Treatment options (start here)
- Footwear: wider, rounder toe box with softer uppers over the bunion; lower heels
- Skin and spacing: soft bunion sleeves/gel shields to reduce rubbing; slim toe spacers to keep toes apart (if comfortable)
- Strength/mobility: gentle big‑toe mobilisation, towel scrunches, short‑foot drills, calf stretches to improve push‑off control
- Training habits: reduce long firm‑surface walks during flares; build distance gradually
- Insoles: orthotic insoles to reduce shoe–skin friction at the bunion, offload “transfer” pressure, and make push‑off more evenly shared
How orthotic insoles help bunions
- Reduce rubbing and pressure: a smooth, low‑friction top layer and silicone‑gel forefoot cushioning soften contact around the bunion and under the ball of the foot.
- Offload the lesser metatarsals: a metatarsal support pad placed just behind the ball of the foot encourages slight splay of the metatarsal heads (transverse arch) and shifts peak pressure off the second/third metatarsal heads.
- Support a more even push‑off: a defined arch contour and a cupped heel help you move from heel strike to push‑off more consistently, so less force is shunted into the lesser rays.
Make walking easier. Fit FootReviver Morton’s Neuroma Insoles (trim at the forefoot), pair with wider, softer‑upper shoes, and build wear time gradually. If redness, swelling, or pain persist, speak to a healthcare professional.
For Hammer Toes
Hammer toes: what it is and how it changes pressure
Hammer toes bend at the middle toe joint (proximal interphalangeal, PIP). Claw toes involve extension at the metatarsophalangeal (MTP) joint with flexion at the PIP and distal interphalangeal (DIP) joints. Both increase pressure under the corresponding metatarsal heads and cause rubbing over the toe knuckles. Pain here is driven by focal load and skin irritation. Morton’s neuroma, by contrast, is a nerve issue between two toes (often the third–fourth webspace) with squeeze‑provoked webspace pain and possible shooting into both adjacent toes.
Who’s most at risk and why
- Tapered toe boxes or high heels that keep toes bent and crowd the forefoot
- A relatively long second metatarsal, forefoot instability, or a bunion that reduces big‑toe push‑off
- Muscle imbalance or calf tightness that alters toe control and forefoot loading
- Prolonged walking on firm surfaces in thin or worn footwear
Where it hurts and what to look for
- Pressure pain under specific metatarsal heads (often beneath the bent toe)
- Corns or callus on the tops or tips of the affected toes; rubbing in snug footwear
- Possible burning in a webspace if an interdigital nerve is also irritated
- Reduced toe flexibility or progressive deformity if symptoms persist
Why addressing it early helps
Bent‑toe postures focus load into small areas under the forefoot and increase rubbing over the toe knuckles. As the forefoot pushes off, the metatarsal heads can press closer together and the transverse arch can flatten, narrowing the space between the heads. That raises pressure on the interdigital nerve and may trigger or worsen neuroma‑type symptoms. Early steps that improve load sharing and maintain forefoot space reduce both local skin/joint irritation and the risk of interdigital nerve pain developing alongside.
First steps that help
- Footwear: wider, rounder toe box with soft uppers and adequate toe‑box height; low heels; some forefoot cushioning
- Activity: vary surfaces and break up long firm‑surface sessions; reduce steep uphill efforts during flares
- Mobility/strength: gentle toe‑straightening and spreading drills, towel scrunches, and regular calf mobility to support a smoother roll‑through
How FootReviver orthotic insoles help
- Offload pressure under the metatarsal heads: a metatarsal support placed just behind the ball of the foot reduces peak forces directly under the sore head(s).
- Reduce rubbing and shear: a low‑friction top cover with forefoot cushioning lowers irritation over toe knuckles and under the forefoot, especially in firmer shoes.
- Guide a steadier step and preserve interspace width: a supportive arch and cupped heel promote a consistent roll‑through and encourage slight forefoot splay at push‑off, which helps limit interspace narrowing that can aggravate interdigital nerves.
Practical tip. Fit the insoles and adjust the metatarsal support so its highest point sits just behind—not on—the most sensitive area. Pair with a wider toe box and increase wear time gradually. If a toe becomes rigid or very painful, seek assessment.
For Turf Toe
Turf toe (first MTP sprain): what it is, who gets it, and how to protect the joint
In a normal step, the big‑toe joint (first MTP) bends upwards during push‑off. Turf toe is a sprain of the ligaments and plantar plate of that joint caused by forced upward bending (hyperextension). It often follows a slip, sudden stop/start, or pushing off on a stiff surface. The joint becomes painful and swollen, bending is tender, and many people avoid pushing off through the big toe—making walking awkward.
Who’s most at risk and why
- Field/court sports, sprints, and dance—fast push‑offs on firm surfaces
- Flexible shoes or boots that allow excessive toe bend
- Limited ankle mobility/tight calves, which drive more bend into the big‑toe joint
- Previous first MTP sprain that hasn’t fully settled
Where it hurts and what to look for
- Pain, swelling, and tenderness over the big‑toe joint (top and underside)
- Pain when you push the big toe upwards or try to push off briskly
- Stiffness and a feeling you cannot “toe‑off” properly; pain worse on firm surfaces
- Bruising in more acute injuries; limping if severe
Treatment options (first steps)
- Relative rest/load control: reduce sprinting, cutting, and hills; use flatter, softer surfaces during recovery
- Footwear: a little forefoot stiffness or a mild rocker sole can limit painful bend; avoid very flexible forefoot shoes in the short term
- Mobility/strength: restore big‑toe extension gradually; add calf stretches and foot intrinsic work
- Short‑term measures: ice after activity; simple taping when advised to limit painful end‑range
- Insoles: orthotic insoles to cushion the big‑toe joint at toe‑off and to shift a little pressure away from the joint while you recover
How orthotic insoles help turf toe
- Cushion painful push‑off: silicone‑gel forefoot cushioning softens load under the first MTP during toe‑off, so each step feels less sharp.
- Shift pressure slightly back: a low support just behind the ball of the foot moves part of the push‑off load a little further back, reducing joint stress while ligaments settle.
- Keep the step controlled: a cupped heel and supportive arch help the foot roll forward predictably without forcing the big toe into painful range.
Support recovery from the ground up. Fit FootReviver Morton’s Neuroma Insoles (trim to size), ensure footwear gives the big‑toe joint enough space and modest stiffness, and build wear time gradually. If swelling or pain persists, speak to a healthcare professional.
For Sesamoiditis
Sesamoiditis: what it is, who gets it, how it differs from Morton’s neuroma, and how to reduce big‑toe pressure
Sesamoiditis is irritation of one or both sesamoid bones and the soft tissues under the big‑toe joint (first metatarsophalangeal joint). These small bones assist the big toe during push‑off, so pain is sharply focused directly under the joint and rises with toe‑off or when pressed. Morton’s neuroma, by contrast, involves a nerve between the toes (often the third–fourth webspace) and typically presents as webspace pain brought on by a gentle side‑to‑side forefoot squeeze, sometimes with shooting into both adjacent toes. This distinction matters: sesamoiditis improves when pressure is reduced under the first metatarsal head, whereas a neuroma improves when space is created between the metatarsal heads in the affected webspace. If you avoid loading the big toe, you may shift more load toward the central forefoot, which can narrow the spaces between the metatarsal heads and irritate interdigital nerves over time.
Who’s most at risk and why
- Activities with strong push‑off through the big toe (sprinting, jumping, rapid direction changes in field/court sports, dance) increase load under the sesamoids.
- Frequent hills and repeated starts/stops raise pressure under the big toe, especially on firm ground or in very thin soles.
- Foot mechanics that focus load under the big toe—such as high arches (reduced shock absorption) or a stiff big‑toe joint—concentrate stress on the sesamoids.
- Footwear and calf tightness: thin or worn forefoot cushioning, a history of forefoot injury, and tight calves that limit ankle bend (reduced dorsiflexion) all increase stress under the big toe.
Where it hurts and what to look for
- Point tenderness under the big‑toe joint, worse with toe‑off, stairs, or tip‑toe positions
- Pain on direct pressure to the sesamoid region; possible mild swelling without widespread redness
- Symptoms that intensify on firm ground and ease with forefoot cushioning or a mild rocker
- Secondary discomfort under central metatarsal heads if you change push‑off to avoid the big toe
First steps that help
- Footwear: choose forefoot cushioning and a modest forefoot rocker to reduce big‑toe bend. Avoid very thin or highly flexible forefoot soles during a flare, and ensure the toe box has enough height so the big toe is not compressed.
- Load management: reduce speed work, hill sessions, and time on firm surfaces. Reintroduce these gradually as symptoms settle.
Mobility/strength: use gentle big‑toe extension stretches and calf stretches to improve heel‑to‑toe movement during walking. Add intrinsic foot exercises (for example, towel scrunches) to improve forefoot control and push‑off stability.
- Surfaces: keep to forgiving surfaces at first (grass, track, cushioned indoor floors), then phase back to pavements as comfort allows.
How FootReviver orthotic insoles help (and how they reduce knock‑on forefoot irritation)
- Cushion where it hurts: forefoot cushioning softens impact under the first metatarsal head during stance and push‑off to reduce local irritation of the sesamoids.
- Shift pressure slightly back from the sesamoids: a subtle support placed just behind the ball of the foot reduces end‑range stress at toe‑off without forcing the big‑toe joint.
- Maintain a consistent roll‑through: a supportive arch and cupped heel guide a steadier step so you are less likely to adopt push‑off patterns that overload the central forefoot or crowd interdigital spaces (useful if a neuroma is also symptomatic).
- Reduce rubbing: a low‑friction top cover decreases shear over tender skin under the big‑toe joint.
Practical tip. Fit the insole and check that the highest part of the support sits just behind—not on—the sesamoid area. Pair with footwear that has forefoot cushioning and a mild rocker. Increase wear time over 1–2 weeks and reintroduce hills or speed work gradually. If focal bone tenderness persists or night pain develops, seek assessment to rule out a sesamoid stress injury.
For Second‑Toe Capsulitis / Plantar Plate Strain
Second‑toe capsulitis / plantar plate strain: pinpoint joint pain under the second toe
Second‑toe capsulitis (plantar plate strain) is irritation or small tears in the ligament‑like tissue under the second metatarsophalangeal (MTP) joint. It causes pinpoint pain at the base of the second toe, tenderness when you press the joint line, and pain when the second toe is bent upward; the toe can feel less secure and may begin to drift toward the big toe. This differs from Morton’s neuroma, which produces pain in the webspace between two toes and may trigger tingling or shooting into both toes with a gentle side‑to‑side forefoot squeeze. Capsulitis pain is joint‑centred and typically does not produce those between‑toe nerve symptoms.
Who’s most at risk and why
- Longer second metatarsal (increased lever and pressure under the second MTP)
- Bunion, hammer/claw toe patterns, or forefoot instability raising second‑ray demand
- Heels or long stride/hill work that increase dorsiflexion at the second MTP
- Prolonged time on firm surfaces in thin or worn footwear
Where it hurts and what to look for
- Pinpoint tenderness under the base of the second toe; swelling is possible
- Pain with toe‑up bending and during push‑off; callus under the second head
- Occasional secondary soreness between the toes if nearby nerves are irritated by load shift
First steps that help
- Footwear: roomier toe box with some forefoot cushioning; avoid high heels during a flare
- Activity: reduce steep hills, fast push‑offs, and long firm‑surface days; rebuild gradually
- Mobility/strength: gentle calf mobility and forefoot control work to improve roll‑through
How FootReviver orthotic insoles help
- Offload the second MTP: a metatarsal support positioned just behind the ball of the foot reduces peak pressure under the second head.
- Share load and reduce shear: increased midfoot contact and a low‑friction, cushioned forefoot spread pressure more evenly and calm joint irritation.
- Steady late stance: a supportive arch and cupped heel guide a consistent roll‑through so you are less likely to overload the second ray or irritate nearby interdigital nerves.
Practical tip. Position the metatarsal support just behind—not on—the sore joint; build wear time gradually.
For Metatarsal Fractures (Acute/Traumatic)
Metatarsal fractures (acute/traumatic): what to expect, who’s at risk, and how to protect the forefoot
An acute metatarsal fracture is a break in one of the long bones in the front of the foot after a twist, a fall, or a heavy object landing on the foot. Pain is immediate, sharp, and fixed to one exact spot, with swelling and bruising typically appearing within hours. This differs from a metatarsal stress injury, where pain develops gradually with increasing distance or time on your feet and often includes pain with hopping or night ache. It also differs from Morton’s neuroma: fracture pain is bone‑focused rather than in the webspace between two toes. A side‑to‑side forefoot squeeze may be painful in a fracture, but it usually does not produce the characteristic between‑toe electric symptoms or palpable click (Mulder sign) seen with a neuroma.
Who’s most at risk and why
- Falls, mis‑steps, dropped objects, or forced forefoot twist
- Contact sports or heavy/awkward loads at work
- Footwear with minimal protection on firm or irregular surfaces
- Bone‑health factors (reduced bone density) that increase fracture risk
Where it hurts and what to look for
- Sudden, focal pain over a metatarsal shaft or head after a clear incident
- Swelling and bruising developing over hours; pain on weight bearing
- Marked tenderness on direct palpation of the bone; possible deformity in displaced fractures
First steps that help (follow clinical advice first)
- Protection/immobilisation: boot, stiff‑soled shoe, or casting as advised; non‑ or partial‑weight bearing initially
- Symptom control: elevation in the early phase; gradual load progression only when allowed
- Footwear: when cleared to walk, use supportive shoes with forefoot cushioning and a wider base
How FootReviver orthotic insoles help (when weight bearing is allowed)
- Cushion and spread load: forefoot cushioning softens impact on firm surfaces and distributes pressure away from the injured ray.
- Shift pressure slightly back: low support just behind the ball of the foot reduces focal push‑off stress near the healing site.
- Guide comfortable steps: a cupped heel and supportive arch encourage a predictable roll‑through, helping you avoid overloading adjacent metatarsal heads during return to walking.
Practical tip. Begin using insoles when your clinician allows weight bearing. Check forefoot comfort, and increase wear time gradually in line with the healing timeline.
For Metatarsal Stress Injury (Reaction or Stress Fracture)
Metatarsal stress injury (reaction or stress fracture): gradual bone overload in the forefoot
A metatarsal stress injury develops when repeated loading exceeds the bone’s repair capacity, progressing from stress reaction to stress fracture. Onset is gradual and distance‑ or time‑related. Pain is very focal over the bone and increases with impact; night ache can occur. This contrasts with acute fractures (sudden incident, early bruising/swelling) and with Morton’s neuroma (between‑toe nerve pain with squeeze‑provoked, electric‑type symptoms rather than a single pinpoint bony spot).
Who’s most at risk and why
- Sudden increases in walking/running, hills, or firm‑surface time; limited recovery between sessions
- Thin or worn soles; minimal forefoot cushioning
- Foot shape factors (long second metatarsal), low bone density, prior forefoot injury
- High step counts or occupational load without adequate pressure sharing
Where it hurts and what to look for
- Localised tenderness along a metatarsal shaft or head; pain with hopping or forefoot impact
- Symptoms rise with distance/pace and ease with offloading; swelling may be mild or absent early
- Later, compensations can create new hotspots under adjacent metatarsal heads
First steps that help (follow clinical guidance)
- Load modification: reduce or pause impact loading; graded return as symptoms settle
- Protection: stiff‑soled shoe or boot as advised; monitor night pain and hop pain
- Footwear: when cleared for progression, use supportive shoes with adequate forefoot cushioning
How FootReviver orthotic insoles help (as activity resumes)
- Cushion and distribute: forefoot gel zones reduce impact and spread pressure so no single head is over‑stressed.
- Subtle offload: low support just behind the ball of the foot shifts part of push‑off away from the injured site.
- Consistent mechanics: a cupped heel and supportive arch promote a controlled roll‑through, limiting compensations that can overload adjacent rays or irritate interdigital nerves.
Practical tip. Introduce insoles once weight‑bearing and walk progression can be done; increase wear time and activity in small steps, guided by symptoms and clinical advice.
For Tarsal Tunnel Irritation
Tarsal tunnel irritation: inner‑ankle nerve compression with tingling/burning into the sole
Tarsal tunnel irritation involves compression of the posterior tibial nerve behind the inner ankle. Symptoms include tingling, burning, or numbness that begin near the inner ankle and radiate into the sole. This differs from Morton’s neuroma, which is usually localised between two toes with squeeze‑provoked pain in a single webspace rather than a broader nerve distribution.
Who’s most at risk and why
- Flat feet/overpronation increasing strain through the tunnel
- Long periods of standing/walking on firm surfaces in unsupportive footwear
- Swelling or tight straps near the inner ankle that reduce tunnel space
- Prior ankle injury or restricted ankle mobility
Where it hurts and what to look for
- Tingling or burning starting at the inner ankle and spreading into the arch/forefoot
- Symptoms that rise with fatigue or prolonged standing and settle with rest
- Occasional altered sensation under the foot rather than focal metatarsal‑head pain
First steps that help
- Footwear: stable heel counter, supportive midfoot, and adequate cushioning
- Activity: break up long standing; vary surfaces; address calf and ankle mobility limits
- Load control: reduce tasks that force prolonged inward roll during a flare
How FootReviver orthotic insoles help
- Support the arch and steady the heel: a defined arch contour and cupped heel reduce excessive inward roll that can increase tunnel tension.
- Soften repetitive load: cushioning under heel and forefoot reduces impact that keeps the nerve irritable.
- Improve step consistency: a supportive contour encourages a controlled roll‑through, limiting compensations that might also irritate interdigital nerves at the forefoot.
Practical tip. Combine insoles with a gradual mobility and strength plan for calves and ankle as advised.
For Interdigital Bursitis
Interdigital bursitis: aching or “fullness” between metatarsal heads
Interdigital bursitis is inflammation of a small fluid‑filled sac (bursa) between metatarsal heads caused by local pressure and shear. It typically feels like aching or a sense of fullness in the webspace with tender swelling. Unlike Morton’s neuroma, it is less likely to produce electric, shooting pain into two toes with a forefoot squeeze.
Who’s most at risk and why
- Narrow or tapered toe boxes that crowd the metatarsal heads
- Thin or worn forefoot cushioning on firm surfaces
- Repetitive forefoot loading or toe deformities increasing local shear
Where it hurts and what to look for
- Webspace tenderness and possible mild swelling
- Discomfort that rises with tight footwear and eases when the forefoot can spread
- Sometimes coexists with neuroma‑type symptoms if the nerve is also irritated
First steps that help
- Footwear: wider, rounder toe box; softer uppers over the forefoot; forefoot cushioning
- Activity: reduce long firm‑surface sessions during a flare; vary pace and surfaces
How FootReviver orthotic insoles help
- Create space at the ball of the foot: a metatarsal support positioned just behind the metatarsal heads encourages slight splay, reducing local crowding in the webspace.
- Reduce rubbing and pressure: a low‑friction top cover and cushioned forefoot lower shear and contact stress over the inflamed bursa.
- Guide even loading: a supportive arch and cupped heel help you roll forward in a controlled way, limiting recurrent focal pressure that can also aggravate interdigital nerves.
Practical tip. Ensure the metatarsal support sits just behind—not on—the tender webspace; increase wear time gradually.
For MTP Joint Synovitis or Osteoarthritis
MTP joint synovitis or osteoarthritis: when toe joints are the source of forefoot pain
Inflammation (synovitis) or cartilage wear (osteoarthritis) affecting one or more metatarsophalangeal (MTP) joints causes joint‑centred pain, stiffness, and swelling. Symptoms are typically reproduced by bending the affected toe or pressing directly on the joint line. This differs from Morton’s neuroma, which produces pain between two toes with squeeze‑provoked, nerve‑type symptoms rather than joint‑line tenderness.
Who’s most at risk and why
- Repetitive forefoot bending (stairs, hills, sprinting) increasing MTP load
- Foot shapes that raise focal pressure (long second metatarsal, bunion, hammer/claw toes)
- Inflammatory arthritis or prior joint injury
- Long periods on firm surfaces in worn or thin‑soled footwear
Where it hurts and what to look for
- Soreness over the involved MTP joint(s), possible swelling and morning stiffness
- Pain with deep toe bend at push‑off or when the joint is pressed
- Secondary discomfort under adjacent metatarsal heads from altered push‑off
First steps that help
- Footwear: forefoot cushioning and a mild rocker to limit painful end‑range; adequate toe‑box height
- Activity: reduce long hill/interval sessions and prolonged firm‑surface time; vary pace and surfaces
- Mobility/strength: gentle calf mobility and foot intrinsic exercises to improve roll‑through
How FootReviver orthotic insoles help
- Reduce joint impact: forefoot cushioning lowers contact stress during stance and push‑off.
- Share load away from the sore joint: supportive contour increases midfoot contact so less force concentrates at one MTP.
- Subtle pressure shift: a metatarsal support set just behind the ball of the foot moves peak pressure slightly back and may reduce interspace crowding that can irritate interdigital nerves.
Practical tip. Pair insoles with footwear that allows the forefoot to roll without forcing deep toe bend.
For Forefoot Fat‑Pad Thinning (Atrophy)
Forefoot fat‑pad thinning (atrophy): reduced natural cushioning under the metatarsal heads
Age‑ or load‑related thinning of the protective fat pad under the metatarsal heads reduces shock absorption. Pain is broader across the ball of the foot and is most noticeable on firm floors. This differs from Morton’s neuroma, which produces more localised, between‑toe pain with nerve‑type symptoms and squeeze‑provoked discomfort in one webspace.
Who’s most at risk and why
- Age‑related tissue changes and long years on firm surfaces
- Repeated forefoot loading with thin or worn soles
- Foot shapes that focus pressure under specific metatarsal heads
Where it hurts and what to look for
- Diffuse tenderness across the forefoot rather than one pinpoint spot
- Callus build‑up over several metatarsal heads
- Symptoms increase with firm surfaces and thin cushioning; ease with softer set‑ups
First steps that help
- Footwear: generous forefoot cushioning and a wider, rounder toe box
- Activity: alternate surfaces, add short breaks to long standing or walking
- Foot care/strength: gentle calf mobility and foot intrinsic work for improved roll‑through
How FootReviver orthotic insoles help
- Replace lost cushioning: forefoot gel zones soften contact and reduce the bruise‑like feel on firm ground.
- Spread pressure more evenly: supportive contour increases midfoot contact so less force concentrates at individual heads.
- Reduce shear: a low‑friction top cover limits rubbing across tender skin and can also lessen interspace irritation when nerves are sensitive.
Practical tip. If one head remains sore, fine‑tune metatarsal support position so the high point sits just behind—not on—the painful area.
For Gout at the Big‑Toe Joint (First MTP)
Gout at the big‑toe joint: acute first‑MTP inflammation with joint‑centred pain
Gout is inflammation caused by uric acid crystals (monosodium urate) building up inside a joint—most often the big‑toe joint (first MTP). A flare usually comes on suddenly with severe pain, heat, redness, and swelling in that single joint, often at night. This differs from Morton’s neuroma, which causes pain between two toes with nerve‑type symptoms (tingling or shooting) rather than an acutely inflamed, swollen joint.
Who’s most at risk and why
- Personal or family history of gout; metabolic or medication factors
- Previous first‑MTP flares or joint damage
- Dietary and health triggers identified by your clinician
Where it hurts and what to look for
- Severe tenderness at the big‑toe joint with warmth, redness, and swelling
- Pain with any contact or movement of the joint
- Limited tolerance for closed, snug footwear during a flare
First steps that help
- Medical assessment for diagnosis and flare management
- Footwear: soft, roomy toe box to reduce joint contact; cushioned sole
- Activity: reduce loading until the flare settles; then rebuild gradually as advised
How FootReviver orthotic insoles help
- Ease contact discomfort: a cushioned forefoot and low‑friction top cover reduce rubbing during and after a flare.
- Support controlled walking: a steady roll‑through helps you resume activity more comfortably as inflammation resolves.
- Prevent secondary overload: supportive contour helps avoid shifting excessive pressure to the central forefoot, which could irritate interdigital nerves.
Important. Insoles improve comfort but do not treat the underlying cause. Follow medical advice for gout management and prevention.
For Peripheral Neuropathy (Comfort Support)
Peripheral neuropathy: widespread burning, tingling, or numbness in the feet
Peripheral neuropathy involves nerve dysfunction causing burning, tingling, or numbness in a diffuse, often symmetrical “stocking” distribution across the feet. Symptoms are broader than Morton’s neuroma, which is usually localised to one webspace between two toes with squeeze‑provoked pain and nerve‑type sensations in adjacent toes.
Who’s most at risk and why
- Specific medical conditions, treatments, or nutritional factors identified by a clinician
- Long‑standing pressure or repetitive loading on firm surfaces
- Reduced protective sensation increasing risk of pressure areas
Where it hurts and what to look for
- Symptoms in both feet or across a large area of the sole rather than one webspace
- Possible sensitivity to friction and pressure from seams or hard insoles
- Balance or awareness of foot position may be reduced in some cases
First steps that help
- Medical assessment to address underlying causes and risk factors
- Footwear: soft, seamless, and roomy forefoot with consistent cushioning
- Activity: vary surfaces; use pacing to limit prolonged standing on firm ground
How FootReviver orthotic insoles help (comfort support)
- Cushion and protect: forefoot and heel cushioning reduces pressure points and friction across sensitive skin.
- Even out loading: supportive contour helps distribute force more consistently to reduce repeat stress on the same areas.
- Reduce secondary forefoot irritation: low‑friction top cover and metatarsal support (when appropriate) can lessen rubbing and interspace pressure that may aggravate interdigital nerves.
Note. Insoles improve comfort and protection but do not treat the underlying neuropathy. Use them alongside clinical guidance.
For Morton’s Toe (Long Second Metatarsal)
Morton’s toe / metatarsal parabola variation
Morton’s toe describes a forefoot shape where the second metatarsal is relatively long. It loads earlier and carries more pressure at push‑off, especially under the second (and often third) metatarsal heads. Pain is primarily load‑driven beneath these heads. This differs from Morton’s neuroma, which is a nerve‑related pain between two toes, commonly in the third webspace, often reproduced by a side‑to‑side forefoot squeeze. Over time, high central pressure can narrow the interspaces and increase the likelihood of interdigital nerve irritation.
Who’s most at risk and why
- Inherited forefoot shape with a long second metatarsal
- Thin forefoot cushioning, narrow toe boxes, or tapered shoes
- Training increases, hills, forefoot‑dominant drill work, or prolonged firm‑surface time
- Coexisting bunion or hammer toes that alter push‑off sharing
Where it hurts and what to look for
- Soreness and callus under the second/third metatarsal heads, worse on firm ground
- Pain that rises with longer distance or faster pace and eases when pressure is shared
- Occasional between‑toe discomfort if a nearby interdigital nerve becomes irritable
First steps that help
- Footwear: wider, rounder toe box with forefoot cushioning; modest forefoot flex or slight rocker to reduce focal loading
- Activity: reduce steep hills and long firm‑surface days during flares; vary surfaces
- Mobility/strength: calf mobility and intrinsic foot control to improve load transfer
How FootReviver orthotic insoles help
- Move pressure slightly back: a metatarsal support positioned just behind the ball of the foot shifts part of the load away from the long second head.
- Spread and soften: increased midfoot contact and a low‑friction, cushioned forefoot reduce rubbing and focal pressure that can irritate sensitive joints and interdigital nerves.
- Promote consistent roll‑through: a supportive arch and cupped heel help share push‑off across more metatarsal heads, reducing recurrent hotspots.
Practical tip. Align the metatarsal support just behind—not on—the most tender area; reassess comfort over a 1–2‑week break‑in period.
For Achilles Tendonitis
Achilles tendinopathy: what it is, who’s at risk, and how to improve comfort
In a normal gait, the Achilles tendon stores and releases energy as you move from landing to push‑off. Achilles tendinopathy is irritation of the tendon at its mid‑portion or where it attaches to the heel bone (calcaneus). It often follows sudden increases in running or hill work, frequent firm‑surface sessions, or footwear changes that alter heel‑to‑toe drop. Pain and stiffness are most noticeable with first steps after rest and at the start of activity.
Who’s most at risk and why
- Runners/walkers increasing speed, hills, or total time too quickly
- Tight calves (reduced ankle dorsiflexion); high‑ or very low‑drop shoes
- Foot posture factors (flat feet or high arches) that alter load through mid‑stance
- Prior Achilles injury; reduced calf/hip strength
Where it hurts and what to look for
- Pain/stiffness at the back of the heel or lower calf; morning stiffness that eases with gentle movement
- Soreness that returns after longer activity or firm‑surface sessions
- Tenderness to pinch along the tendon or at its attachment; sometimes mild swelling or crepitus
Treatment options (start here)
- Relative rest and graded loading: reduce speed/hills and firm‑surface time; follow a structured calf‑strengthening programme
- Footwear: secure, supportive shoes with adequate heel‑to‑toe drop during rehab; replace worn soles
- Mobility: daily calf stretches if ankle dorsiflexion is limited
- Short‑term measures: ice after activity; simple taping when advised
- Insoles: orthotic insoles to reduce heel impact, improve mid‑stance control, and prevent compensatory forefoot overload
How orthotic insoles help Achilles tendinopathy
- Cushion and seat the heel: a cushioned, cupped heel reduces the jolt at landing (heel strike) and positions the heel consistently, easing tendon tension.
- Support mid‑stance: a defined arch contour steadies the foot as you load it, so the calf and tendon don’t fight excessive inward roll or lateral wobble.
- Avoid forefoot overload: if you avoid heel contact, subtle forefoot support and cushioning help keep push‑off pressure shared while the tendon settles.
Use insoles alongside a structured rehab plan. Fit FootReviver Morton’s Neuroma Insoles (trim to size), ensure the heel feels seated and the arch supported, and build wear gradually. If pain persists or worsens, speak to a healthcare professional.
For Shin Splints
Shin splints (medial tibial stress): what it is, who gets it, and how to reduce load on the shin
In a normal step, your lower‑leg muscles help control how the shin (tibia) loads and unloads. Shin splints (medial tibial stress syndrome) occur when repeated traction and bending forces along the inner border of the tibia exceed what the bone and its lining can tolerate. It usually follows a quick rise in training volume or intensity, frequent sessions on firm ground, or footwear/mechanics that allow too much inward roll (pronation).
Who’s most at risk and why
- Runners and brisk walkers increasing distance, speed, hills, or frequency too fast
- New standing or walking‑heavy roles on firm surfaces in unsupportive shoes
- Flatter feet or prolonged inward roll, tight calves, prior shin splints
- Reduced hip strength/control; very worn footwear
Where it hurts and what to look for
- Diffuse ache or tenderness along the inner border of the shin (lower two‑thirds)
- Pain that starts after exercise, then during exercise if you keep loading; eases with rest
- Tight calves and a “bruised” feel along the inner shin after longer sessions
- Red flags: focal point tenderness, night pain, sharp hop pain—seek assessment (possible stress fracture)
Treatment options (start here)
- Training changes: reduce frequency/distance/pace; add rest days; rebuild gradually
- Surfaces/footwear: mix softer surfaces; supportive footwear with adequate cushioning and heel control
- Strength/mobility: calf stretches, ankle mobility, and progressive calf/hip/core strengthening
- Short‑term comfort: ice after activity; taping when advised
- Insoles: orthotic insoles to reduce impact, moderate inward roll, and improve landing consistency
How orthotic insoles help shin splints
- Absorb impact: silicone‑gel zones under the heel and forefoot reduce shocks that travel up the shin on firm surfaces.
- Moderate inward roll: a supportive arch contour limits excessive pronation and tibial rotation during mid‑stance, reducing traction on the tibial border.
- Improve landing consistency: a cupped heel steadies heel strike so each step starts from a more controlled position—useful as you rebuild volume.
Make a sensible start. Fit FootReviver Morton’s Neuroma Insoles (trim to size), pair with supportive footwear, and increase time and distance gradually. If pain persists—or if you suspect a stress fracture—speak to a healthcare professional.
For Knee Pain
Knee pain: patterns, contributing factors, and how neuroma‑driven gait changes play a part
Knee pain doesn’t come from one place. Muscle imbalance, meniscal irritation, cartilage wear, arthritis, and previous injury can all play a role. Alongside these, there’s a link that’s easy to miss: pain under the ball of the foot that changes how you walk. Morton’s neuroma is irritation and thickening of a small nerve between the metatarsal bones, usually between the third and fourth toes (common plantar digital nerve in the third intermetatarsal space). The familiar burning, “pebble under the foot” feeling at push‑off nudges you to move differently—and those small changes can increase stress at the knee.
How Morton’s neuroma alters gait and increases knee load
- Shorter steps and early heel rise: lifting the heel sooner limits time on the sore spot. This raises pressure behind the kneecap on slopes and stairs (higher patellofemoral joint reaction force).
- “Dodging” the hotspot: tipping weight to the outer edge or rolling inward earlier adds twist through the shin (tibial rotation) and can increase inner‑knee compression (medial compartment contact stress).
- Less big‑toe use: avoiding toe bend weakens the arch‑tightening effect (windlass mechanism), allowing more inward roll (pronation). That can nudge kneecap tracking and irritate the front of the knee.
Other contributors (not an exhaustive list)
- Training spikes, hills/stairs, long descents; deconditioning
- Hip/glute and quad weakness; tight calves; movement control issues (dynamic valgus)
- Worn or unsupportive footwear
- Previous knee injury, meniscal tears, or osteoarthritis
What to look for
- Ache around or behind the kneecap on stairs, squats, or rising from a chair
- Inner‑knee ache or stiffness with longer walking or standing
- Symptoms that ease when forefoot pain is offloaded and push‑off feels normal again
- Red flags: giving‑way, locking, or marked swelling after minor activity—seek assessment
What helps first
- Activity: temporarily trim hills/stairs; add short breaks to long standing; rebuild volume gradually
- Strength/mobility: hip/glute and quad strengthening, controlled step‑downs, regular calf stretches
- Footwear: supportive, cushioned shoes with a firm heel counter; replace very worn soles
- Insoles: orthotic insoles to soften impact and steady the foot; if forefoot pain is present, offload the ball of the foot so push‑off is comfortable and natural again
How orthotic insoles help when ball‑of‑foot pain is part of the picture
- Restore comfortable push‑off: a metatarsal support placed just behind the ball of the foot (proximal to the metatarsal heads) gently spreads the bones and eases pressure on the irritated nerve; forefoot silicone‑gel cushioning softens contact so you don’t twist or guard at the knee.
- Reduce shocks: silicone‑gel zones at the heel and forefoot lower impact each step, easing load transmitted to the knee.
- Keep the leg aligned: a supportive arch and cupped heel guide the foot from heel strike to mid‑stance with less excess inward roll (pronation), reducing irritating peaks at the kneecap and inner knee.
Take a practical step. Fit FootReviver Morton’s Neuroma Insoles (trim the forefoot to size), wear supportive footwear, and increase walking time gradually. If symptoms persist or red flags appear, speak to a healthcare professional.
For Hip Pain
Hip pain: impact, alignment, and how neuroma‑related changes can aggravate symptoms
In a normal step, impact is absorbed at the foot and ankle, forces transfer smoothly through the leg, and the pelvis stays level. Hip pain often worsens when impact is high and small alignment changes add up—long days on firm surfaces, minimal/worn footwear, reduced hip strength, or compensating for another sore area (knee, foot). Typical patterns include outer‑hip pain over the greater trochanter (lateral hip) and groin stiffness/ache with longer walking (hip joint overload).
How Morton’s neuroma can contribute
When a neuroma in the forefoot makes push‑off painful, you may shorten stride, avoid toe‑off on the affected side, or walk more on the outer edge. These changes reduce normal hip extension and can increase pelvic drop, asking more of the hip abductors and lateral tissues. Over time—especially on pavements and other firm surfaces—these compensations can aggravate lateral hip pain or groin symptoms.
Who’s most at risk and why
- Long periods walking/standing on firm surfaces in thin or worn footwear
- Sudden increases in hills/stairs or speed without recovery
- Reduced hip/glute strength, tight calves, and foot postures that change leg alignment
- Prior hip or lower‑limb injury
Where it hurts and what to look for
- Outer‑hip tenderness lying on that side or after long walks (lateral hip)
- Groin ache or stiffness with prolonged standing/walking; “start‑up” pain easing as you warm up
- Symptoms that rise on firm surfaces and settle with softer footwear or rest
- Red flags: night pain, mechanical locking/catching, or true giving‑way—seek assessment
Treatment options (first steps)
- Activity changes: break up long standing; vary pace/surfaces; build distance gradually
- Strength/mobility: focused hip/glute strengthening, step‑down control, and calf flexibility
- Footwear: cushioned, supportive shoes with secure heel counters; replace worn soles
- Insoles: orthotic insoles to reduce impact and promote a more consistent foot motion—plus offload forefoot pain from a neuroma so you don’t keep altering your hip mechanics
How orthotic insoles help when hip pain is linked to a neuroma
- Make toe‑off comfortable again: a metatarsal support just behind the ball of the foot and forefoot silicone‑gel cushioning reduce forefoot sting, so you can stride out and extend the hip more naturally.
- Soften hard landings: silicone‑gel cushioning at the heel and forefoot reduces repetitive shocks that travel up to the hip on firm surfaces.
- Promote a more consistent roll‑through: a supportive arch and cupped heel encourage a smoother progression from heel strike to mid‑stance, helping limit the small alignment changes that irritate hip tissues.
Begin with the basics. Fit FootReviver Morton’s Neuroma Insoles (trim to size), wear supportive footwear, and increase walking time gradually. If hip pain persists or night pain appears, speak to a healthcare professional.
For Back Pain and Poor Posture
Back pain and posture: impact control, step consistency—and the role of neuroma‑driven compensation
On a typical day, your feet absorb and smooth out impact so your legs and spine don’t take every jolt. Back discomfort often builds when you spend long periods on firm surfaces in thin or worn footwear, or when small leg/pelvis alignment changes persist as you fatigue. Symptoms tend to rise across a shift or a longer walk and ease with breaks or more cushioned shoes.
How Morton’s neuroma can contribute
If a neuroma makes the front of your foot sore, you may shorten your stride, spend longer with both feet on the ground, or walk unevenly to avoid the hotspot. That can increase vertical loading, reduce normal shock absorption at push‑off, and introduce a slight asymmetry from step to step. Over hours on firm surfaces, those changes can increase low‑back muscle fatigue and joint irritation.
Who’s most at risk and why
- Jobs that involve prolonged standing/walking on firm surfaces
- Minimal or very worn footwear with little cushioning or heel control
- Reduced hip/glute strength and tight calves, which change step mechanics
- Prior back issues that flare with repetitive loading
Where it hurts and what to look for
- Dull low‑back ache that builds over the day; stiffness after long standing/walking
- Relief with breaks, softer footwear, or walking on more forgiving surfaces
- Symptoms that flare when fatigued or when shoes are worn down
- Red flags: progressive pain with night symptoms, leg weakness/numbness—seek assessment
Treatment options (start here)
- Breaks and movement: alternate standing with short walks; use anti‑fatigue mats if available
- Strength/mobility: hip/glute/core strengthening and regular calf stretches
- Footwear: well‑cushioned, supportive shoes with secure heel counters; replace worn soles
- Insoles: orthotic insoles to soften impact and promote a more predictable step—and, if a neuroma is present, to reduce forefoot pain so you don’t have to walk unevenly
How orthotic insoles help when back pain is linked to a neuroma
- Reduce ground shocks: silicone‑gel cushioning under the heel and forefoot softens repeated impacts on firm surfaces, lowering the load passed up the chain.
- Support a more even stride: a metatarsal support just behind the ball of the foot and forefoot gel cushioning reduce neuroma pain, so you don’t have to shorten or guard the step on one side.
- Guide a consistent step: a supportive arch and cupped heel help your foot move from heel strike to mid‑stance in a more predictable way, which can ease small leg/pelvis alignment changes that contribute to back ache.
Start now. Fit FootReviver Morton’s Neuroma Insoles (trim the forefoot to size), choose supportive footwear for longer standing, and build wear gradually. If back pain persists—or you develop leg numbness or weakness—speak to a healthcare professional.















by Connie
A good pair of insoles!!! They provide lots of support and cushioning and have helped a great deal with easing my mortons neuroma. Buying more pairs as we speak 😎
by Caroline Todd
Of all the insoles I have purchased these are the best, cushions my mortons neuroma, will definitely buy more.
by Emily
I got them for my elderly mom who’s been dealing with foot pain for a while now due to Morton’s neuroma. She’s tried everything to get some relief, and nothing seemed to work until she tried these insoles.
They’re sturdy and well-made, she’s been using them for about six weeks now, and they’re still in great shape. Comfort-wise, she describes them as walking on a cloud. They fit nicely in her shoes and provide the support she needs for her foot. These insoles have given her the relief she was looking for. She can now walk comfortably without grimacing in pain. Quality and effectiveness combined in one. And for the price, they’re a steal!
In short, these insoles have been a significant help for my mom. She couldn’t be happier with them, and she highly recommends them to anyone dealing with foot pain.
by Bob Thompson
I’ve been dealing with Metatarsalgia and Morton’s Neuroma for quite some time now. The pain and discomfort were something of a constant companion until I stumbled upon these insoles. The arch and heel support they provide is impressive. They’ve made walking much less painful for me and my feet feel more aligned and balanced. These insoles were easy to trim to my shoe size and they fit perfectly into my everyday shoes. They deliver an excellent stability, especially for my sprained ankle. Feels like a cushion protecting my feet from the harsh ground and jolts. My feet feel less strained and the pain has been significantly reduced. A little improvement on the toe support would make this product perfecto!!! I’m glad I found these insoles, they’ve really helped a heck of a lot!
by Ayesha
So relieved that I found these gel insoles! I’ve been dealing with Morton’s neuroma for months, and standing at work was PURE TORTURE. I slipped these into my shoes and wow! What a difference. No more wincing with every step. The cushioning is just perfect. My feet finally feel free. Can’t believe it! 🎉
by Richard Greene
Putting these insoles in my shoes made a HUGE difference! My Morton’s Neuroma was KILLING me! My feet feel so much better now. They’re lightweight, fit great in my shoes, and the support is TOP-NOTCH. HIGHLY RECOMMENDED!
by John Brown
I’ve been dealing with Morton’s neuroma and metatarsalgia for ages, and these insoles are a breath of fresh air. The shock absorption is impressive and they’re lightweight which makes them comfortable for daily use.
by TOM SMITH
WOW, THESE INSOLES ARE A GAME-CHANGER! I CAN’T BELIEVE HOW MUCH DIFFERENCE THEY MAKE. THE PAIN IN MY FEET IS ALMOST GONE, AND I CAN STAND FOR HOURS WITHOUT PROBLEMS. IF YOU SUFFER FROM MORTON’S NEUROMA, GET THESE NOW!
by Fatima
These insoles are a MUST for anyone with foot pain. I bought them for my Morton’s neuroma, and they’ve been a blessing. Walking is now pain-free and enjoyable! The gel provides ample cushioning, reducing the pressure on my foot. I wear them in all my shoes, from work boots to running shoes. Worth every penny. 😊🌟