No products in the cart.
Medical Compression pressure socks for poor circulation
£8.99inc VAT
- 1x Pair of Medical Compression pressure socks for poor circulation expertly crafted using soft, premium materials for the best support, compression and durability
- For both Men & Women
- Available in S/M & L/XL sizes (Knee high length)
- Ideal for people suffering from Poor circulation, Varicose Veins, Deep Vein Thrombosis, Oedema (swollen legs and feet), Raynaud’s Disease, Arthritis, Blisters, Calluses, Morton’s Neuroma, Metatarsalgia, Plantar Fasciitis, Heel Spurs, Achilles tendonitis, Cuboid Syndrome, Ankle sprains and strains, Shin Splints and tired aching legs and feet
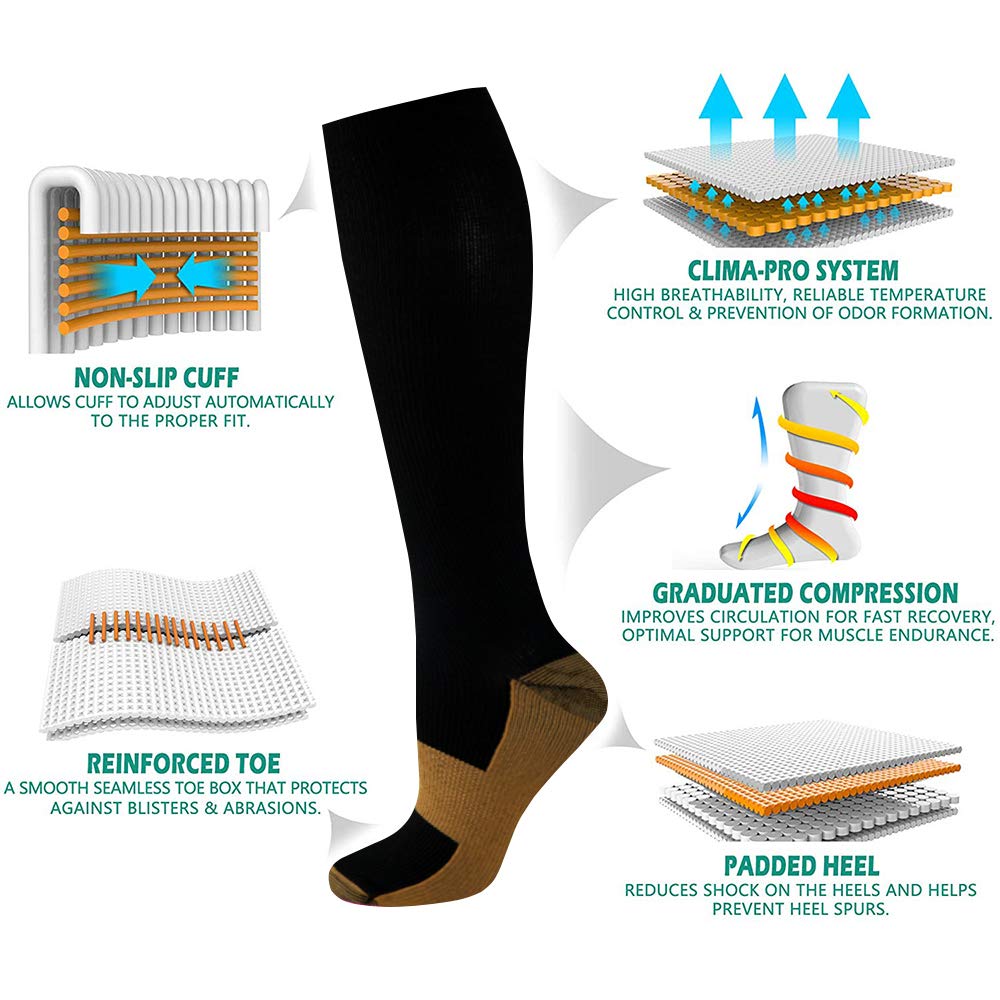
- Features a specially designed cuff that does not dig into your legs or restrict blood flow to your feet when you wear the socks but keeps the socks up and securely in place
- Can be worn for long haul Flights and Travel, Nursing, Pregnancy, Post-op recovery, Exercise and Running
- Provides soothing compression that eases tension in your feet and lower legs and stimulates blood flow to reduce swelling and inflammation, drain excess fluid and ease aches and pains deep within your bones, joints, ligaments and tendons
- Provides support that helps stabilize and ease strain and pressure off your lower legs and feet to help protect you from injury and aches and pain after being on your feet for long periods of time
- The boost in circulation that these socks will give you can help to ease Raynaud’s disease symptoms and promote the healing process and stop muscles fatigue by stimulating your blood vessels and keeping them expanded and the supply of fresh blood flowing to your lower legs and feet
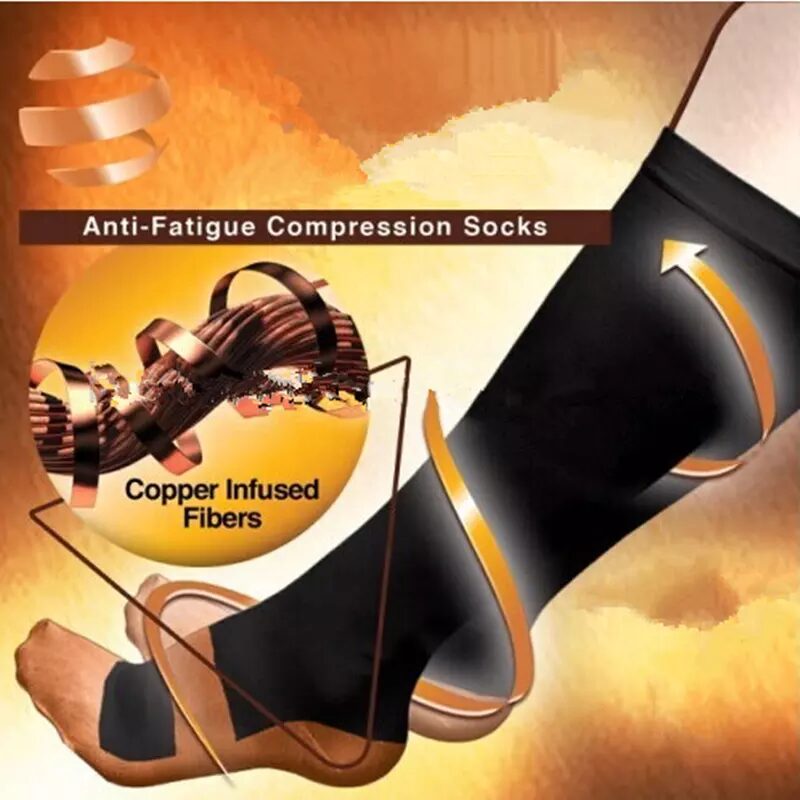
- Infused with copper fibres that help neutralize bacteria and odour to ward off infection, stop skin irritations and keep your feet and lower legs fresh and comfortable though the day
- Includes a full 30-day money back guarantee!
Disclaimer: If you suffer from any sort of medical condition that affects your circulation in your lower limbs please consult your doctor before wearing these pressure socks to make sure that they are right for you and will help with your specific medical needs!
It’s a familiar scenario – you’ve been on your feet all day and now they feel as though they are carrying the weight of the world. Your lower legs are throbbing and your feet are swollen and aching. Your poor circulation is causing you discomfort and you’re longing for relief. Allow us to introduce you to our revolutionary solution – the RevitaFit Medical Compression Pressure Socks.
Feel the Revitalizing Power of RevitaFit Medical Compression Pressure Socks!
If you’re one of the millions who suffer from poor circulation within your lower legs and feet, we’ve got something designed just for you. This revolutionary product is expertly crafted with your comfort, relief, and well-being in mind.
The RevitaFit Medical Compression Pressure Socks are not just your average pair of socks! They offer support and relief, easing strain and pressure off your lower legs and feet. By boosting circulation, they alleviate symptoms of wide range of different conditions. Step into comfort and embrace the healing process with the RevitaFit Medical Compression Pressure Socks. The power to change your life is just a sock away.
What Makes RevitaFit Socks So Special?
Suffering from Varicose Veins, Deep Vein Thrombosis, Oedema, or Raynaud’s Disease? These socks are ideal for you! Even for those dealing with Blisters, Calluses, Morton’s Neuroma, Metatarsalgia, Plantar Fasciitis, Heel Spurs, Cuboid Syndrome, Ankle sprains and strains, Shin Splints, and tired aching legs and feet, RevitaFit socks are a go-to solution.
Knitted from soft, premium materials, these socks provide not only the best support but also standout durability. Men and women alike can enjoy the benefits of these socks in S/M and L/XL sizes, ensuring a perfect fit for a range of individuals.
How do these socks work?
You might be wondering how exactly these socks work. The secret is compression, a proven method to stimulate blood flow and reduce swelling.
The basic principle of compression is simple but ingenious: the socks apply the maximum compression at your ankle, and the pressure gradually decreases as it goes up the leg. Imagine a soft, invisible hand gently squeezing and releasing your leg, encouraging blood to flow back towards your heart. This genius design is backed by a plethora of scientific studies, demonstrating improved blood flow and reduced swelling, both of which are crucial for overall foot health.
So, what does the improved circulation mean for your feet and lower legs? Well, a lot. Your feet carry your body weight all day long, dealing with enormous pressure and tension. When blood circulation is enhanced, it facilitates efficient delivery of oxygen and nutrients to these hardworking muscles, ligaments, and tendons of your feet. This replenishes them, promoting faster recovery, reducing inflammation, and ultimately, alleviating those stubborn aches and pains.
A study in the Journal of Vascular Surgery showed that wearing compression socks such as these significantly increased the velocity of blood flow in the legs, effectively decreasing the risk of blood pooling and clot formation. This is particularly beneficial for people who spend a long time sitting or standing, as their blood circulation is often impacted leading to swollen, achy feet.
But the benefits of wearing these socks are not limited to foot health alone. The positive effects ripple throughout the body, contributing to your overall wellbeing. By reducing the swelling and inflammation in your feet and lower legs, these socks can help you feel more comfortable and energized. A day free from foot pain can increase your mobility, which in turn allows you to lead a more active and fulfilling lifestyle.
Moreover, the reduction in inflammation and the efficient removal of excess fluid, which can often result in edema, means less strain on your cardiovascular and lymphatic systems. This can potentially lower the risk of conditions related to these systems.
Designed to be comfortable to wear all day long!
Made from soft, lightweight materials that is infused with copper fibres. These copper fibres help neutralize bacteria and odour. This helps ward off infection, prevents skin irritations, and keeps your feet and lower legs fresh and comfortable throughout the day.
Another great feature that make these socks so special, is the uniquely crafted cuff that doesn’t restrict blood flow or dig into your legs. Instead, it keeps the socks securely in place, ensuring your comfort throughout the day. That’s not all! These socks are the perfect companion for long-haul flights, travel, nursing, pregnancy, post-op recovery, exercise, and running.
With RevitaFit Medical Compression Pressure Socks, you’re not just investing in a pair of socks, but in a healthier and more comfortable lifestyle. Say goodbye to tired, aching legs, and embrace the soothing comfort of our compression socks. Don’t wait – give your feet the care they deserve, today!
Fast & Secure Checkout Through Paypal
Pay with Paypal the secure payment gateway that accepts all credit and debit cards. Paypal is free and secure and no credit or bank information is ever stored or shared with us.
Fast Dispatch
Enjoy your items soon with quick dispatch via Royal Mail First Class. Expect to have your items between 1-3 days for domestic orders. 7-10 Working days for international orders.
Return Policy – 30 Day Money Back Guarantee
We are so confident that you will just love our product that we offer a full 30 day money back guarantee. In the unlikely event, you are unhappy with your purchase you can simply return it within 30 days for a refund. Please contact us via the form on the contact us page to start your return.
To return an item please send it to: Nuova Health UK, 81 Highfield Lane, Waverley, Rotherham, S60 8AL. Please include a note with your order id so we know who to refund. Please retain your postage receipt as proof of postage. All that we ask is that the item is in the original packaging and unused.





Reviews
There are no reviews yet.