No products in the cart.
Knee High Compression Copper Fit Socks for Men & Women
- Brand: FootReviver
- ( 3 Reviews )Rated 5.00 out of 5 based on 3 customer ratings03
£8.99inc VAT
- 1x Pair of Medical grade Compression Knee High Copper Fit Socks designed to support and ease tired aching feet and legs
- For both Men & Women
- Available in S/M & L/XL sizes
- Machine washable
- Non binding honeycomb top moulds to the exact contours of your legs keeping the socks up and stopping them from moving around whilst wearing them
- Recommended for people suffering from Circulation problems, Deep Vein Thrombosis (DVT), Blood Pooling, Varicose Veins, Raynaud’s disease, Sensitive Feet, Lymphedema, Swollen feet and legs, Plantar fasciitis, Achilles tendonitis or simply tired and aching feet
- Provides targeted and graduated compression to help improve blood circulation to your feet and lower legs
- Designed to reduce swelling and inflammation as well as promote the natural healing process of damaged tissue by providing fresh oxygenated blood to your lower legs
- Features arch and heel support that will help ensure that your feet are properly supported to prevent excessive strain and pressure and shock from causing damage to your feet and stop overuse injuries such as Plantar fasciitis and Achilles tendonitis from occurring when you are on your feet all day
- Made from a high quality blend of copper nylon and spandex material that are breathable with moisture wicking and anti bacterial properties to help keep your feet dry, sweat and odour free
- Smooth padded heel and toes help minimise friction and abrasions protecting your feet from irritation and from blisters and calluses from forming
- Includes a full 30 day money back guarantee!
Please note there is no guarantee of specific results and that the results can vary for this product.
EAN: 5061006075473
SKU:
50615-2
Categories: Compression Socks, Deals, Sale
Tags: Best Choice, Featured, Health, Promotion
Dealing with conditions like varicose veins, muscle fatigue, or poor circulation? Or perhaps you’re looking for extra support during long hours of sitting or standing? Here at NuovaHealth, we may have just the solution you’re searching for: innovative Footreviver Compression Socks.
Designed to provide targeted support and enhance blood flow, these socks can help alleviate discomfort and improve your daily comfort. Before we dive into what makes these compression socks the best choice for you, let’s first explore the benefits of compression therapy and the various situations where you might want to wear compression socks and how they can help.
The Benefits of Compression Therapy
Compression therapy is a time-tested method used to improve blood circulation, reduce swelling, and support muscle function. By applying gentle pressure to your legs, compression socks help your veins work more efficiently, pushing blood back toward your heart and subsequently reducing the risk of blood pooling or clot formation. This can be particularly beneficial for individuals who spend long periods either sitting or standing, as well as those recovering from surgery or managing certain medical conditions.
Why Compression Socks?
- Enhanced Circulation: Compression socks are specifically designed to apply consistent pressure, which encourages blood flow from your lower extremities back to your heart. This alleviates symptoms of poor circulation, such as swelling and discomfort.
- Muscle Support: By providing additional support to your muscles, these socks can reduce muscle fatigue and soreness, making them ideal for athletes or anyone engaged in physical activities.
- Swelling Reduction: Compression socks are highly effective in minimizing edema (swelling) in the lower legs, making them an excellent option for pregnant women or individuals with lymphedema.
Let’s now consider the various situations, injuries, and conditions where wearing a pair of compression socks can be beneficial:
For Plantar Fasciitis
Plantar Fasciitis:
Plantar Fasciitis. For many individuals experiencing foot pain, understanding this condition is essential. This section will explore the specifics of Plantar Fasciitis, its significance, and various treatment options, including the use of compression socks, to offer relief and prevention.
What is Plantar Fasciitis?
Plantar Fasciitis refers to the inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes. This tissue plays a pivotal role in supporting the arch of your foot and absorbing shock as you walk. When it becomes inflamed, it can lead to significant discomfort and pain, particularly in the heel.
In the UK, approximately 10% of the population will experience Plantar Fasciitis at some point in their lives. This statistic underscores just how common and widespread this condition really is.
Affected Body Part
As mentioned, the plantar fascia is situated on the bottom of the foot, extending from the heel to the toes. The inflammation primarily affects the heel area, which can severely impact your mobility and quality of life.
Causes and Risk Factors
Understanding the root causes and identifying those most at risk can help in both treatment and prevention. Here are some contributing factors:
- Overuse and High Impact Activities: Engaging in activities that put a lot of stress on your feet, such as running or dancing, can cause wear and tear on the plantar fascia.
- Age: People between the ages of 40 and 60 are at a higher risk due to the natural wear and tear on the plantar fascia.
- Weight: Excess weight puts additional pressure on your feet, exacerbating the strain on the plantar fascia.
- Foot Mechanics: Flat feet, a high arch, or an abnormal walking pattern can affect the way weight is distributed when you’re standing, adding stress to the plantar fascia.
- Occupational Hazards: Jobs that require long periods of standing or walking on hard surfaces can increase your risk.
Symptoms and Importance of Treatment
Common symptoms include sharp pain in the heel, especially after periods of rest or upon waking up. You might also experience stiffness and tenderness. Ignoring these symptoms can lead to chronic pain and complications such as heel spurs or altered walking patterns, which can cause issues in other parts of the body, like the knees, hips, and back.
Treatment Options
Treating Plantar Fasciitis involves a multifaceted approach:
- Rest and Ice: Reducing physical activity and applying ice can help alleviate inflammation.
- Stretching Exercises: Specific stretches targeting the calf muscles and plantar fascia can promote healing.
- Orthotic Devices: Custom-made or over-the-counter orthotics can provide support and distribute pressure more evenly.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can manage pain and reduce inflammation.
- Physical Therapy: A physical therapist can guide you through exercises that strengthen the lower leg muscles and stabilize your walk.
- Surgery: In severe cases, surgical intervention might be necessary to detach the plantar fascia from the heel bone.
Role of Compression Socks
Among the range of different treatment options, compression socks stand out for their effectiveness in both treating and preventing Plantar Fasciitis. These socks apply graduated pressure to the foot and calf, improving blood circulation and reducing swelling.
How Compression Socks Help
- Improved Blood Flow: By enhancing circulation, compression socks can accelerate the healing process.
- Reduced Swelling: The pressure exerted by the socks helps reduce edema, alleviating pain and inflammation.
- Support and Stability: Compression socks provide additional support to the arch of your foot, reducing strain on the plantar fascia.
- Prevention of Further Injury: By stabilizing the foot and ankle, these socks can help prevent the recurrence of Plantar Fasciitis.
Conclusion
Plantar Fasciitis is a common yet debilitating condition that can significantly impact your daily life. Understanding its causes, symptoms, and treatment options is crucial for effective management and prevention. Among the various treatments, compression socks offer a practical and efficient solution, providing both immediate relief and long-term benefits.
If you’re experiencing symptoms of Plantar Fasciitis, don’t ignore them. Early intervention can prevent complications and ensure a quicker recovery, allowing you to get back on your feet—pain-free.
For Raynaud's Disease
Raynaud’s Disease:
Raynaud’s disease is a condition where the body’s natural response to cold or stress—narrowing of blood vessels—is exaggerated. Normally, the body narrows blood vessels to preserve heat during cold temperatures or in response to stress. However, with Raynaud’s disease, this response can occur excessively even with minimal triggers, leading to significantly reduced blood flow. This can severely affect your toes and feet, causing them to become icy and numb. It’s not just a winter issue, but a potentially chronic condition that can impact you year-round. Let’s delve into the specifics of Raynaud’s disease, focusing on its impact on your lower extremities, and explore how you can manage and mitigate its symptoms.
What is Raynaud’s Disease?
Raynaud’s disease, or Raynaud’s phenomenon, manifests when the small blood vessels in your extremities constrict excessively in response to cold or stress. This vasospasm reduces blood flow, leading to color changes, pain, numbness, and a prickly sensation in the affected areas. When these symptoms occur in your toes and feet, it can significantly impact your daily activities and comfort.
Prevalence and Affected Areas
Raynaud’s disease is more common than you might think. In the UK, it affects approximately 10 million people, with a higher prevalence among women. While it can impact fingers, hands, and ears, we’ll focus on its effects on toes and feet—areas crucial for mobility and balance.
Causes and Risk Factors
Understanding the triggers and risk factors for Raynaud’s disease is key to managing it effectively. Here are some common causes and groups at higher risk:
- Cold Temperatures: Exposure to cold environments can trigger symptoms.
- Stress: Emotional stress can induce vasospasms.
- Gender: Women are more likely to develop Raynaud’s.
- Age: It commonly starts between ages 15 and 30.
- Family History: Genetics play a role.
- Occupational Hazards: Jobs involving repetitive motion or vibrating tools increase the risk.
Symptoms and Importance of Treatment
The hallmark symptoms of Raynaud’s in the toes and feet include:
- Color Changes: Affected areas may turn white, blue, and then red.
- Numbness and Tingling: Reduced blood flow can cause a loss of sensation.
- Pain: Discomfort ranges from mild to severe.
Ignoring these symptoms is risky. Without treatment, prolonged lack of blood flow can lead to ulcers, infections, and, in severe cases, gangrene. Thus, timely intervention is crucial.
Treatment Options
Managing Raynaud’s disease involves several strategies:
- Lifestyle Changes: Dress warmly, manage stress, and avoid smoking.
- Medications: Calcium channel blockers and vasodilators can help improve blood flow.
- Surgical Options: In severe cases, procedures to address nerve issues might be necessary.
- Alternative Therapies: Biofeedback and acupuncture could offer relief.
The Role of Compression Socks
Compression socks can be a game-changer for those with Raynaud’s affecting the feet. These socks apply graduated pressure to your legs and feet, which can:
- Enhance Circulation: By promoting blood flow, they help prevent vasospasms.
- Maintain Warmth: The materials used in compression socks often provide additional insulation.
- Reduce Swelling: They help manage edema, which can exacerbate symptoms.
Technically, compression socks work by applying the most pressure at the ankle, decreasing gradually up the leg. This pressure gradient aids venous return, ensuring blood doesn’t pool in your feet and toes. For Raynaud’s sufferers, this means a reduced chance of blood vessel constriction due to improved overall circulation.
Conclusion
Raynaud’s disease, particularly when it affects your toes and feet, is more than just a nuisance. It’s a condition that requires attention and appropriate management to avoid severe complications. By understanding its causes, recognizing the symptoms, and exploring treatment options—including the use of compression socks—you can take proactive steps to alleviate discomfort and improve your quality of life. Remember, addressing this condition is not just about immediate relief but also about long-term health and well-being. Stay informed, stay warm, and consult healthcare professionals to tailor a management plan that works best for you.
For Neuropathy
Neuropathy in the Toes and Feet:
Neuropathy, particularly peripheral neuropathy affecting the toes and feet, is a pervasive medical condition that warrants serious attention—especially for individuals suffering from diabetes. Imagine losing the ability to feel your toes or experiencing a constant burning sensation in your feet. This is the reality for many people living with neuropathy. But what exactly is this condition, and why is it crucial to manage it effectively?
Peripheral neuropathy is a disorder that occurs when the peripheral nerves, those outside the brain and spinal cord, are damaged. These nerves play a vital role in transmitting signals between the central nervous system and the rest of your body, including your feet and toes. When these pathways are disrupted, it can lead to a range of uncomfortable and often debilitating symptoms.
The Prevalence of Neuropathy
In the United Kingdom, approximately 2-3% of the population is affected by peripheral neuropathy, with a higher prevalence among older adults and those with chronic conditions like diabetes. For diabetics, neuropathy is particularly common, affecting up to 50% of individuals with long-standing diabetes.
The Impact on Your Feet and Toes
Neuropathy primarily impacts the sensory nerves in your extremities, resulting in symptoms such as numbness, tingling, burning sensations, or sharp pain in your feet and toes. This can make simple tasks like walking or even standing extremely painful and challenging.
Causes and Risk Factors
Understanding the root causes and risk factors of neuropathy is essential for prevention and management. The most common causes include:
- Diabetes: High blood sugar levels can damage nerves over time.
- Chronic Alcoholism: Excessive alcohol consumption can lead to nutritional deficiencies that harm nerve health.
- Autoimmune Diseases: Conditions like lupus or rheumatoid arthritis can cause the immune system to attack nerve tissues.
- Infections: Certain infections, such as Lyme disease or HIV, can damage nerves.
- Trauma: Physical injury to the nerves can result in neuropathy.
- Vitamin Deficiencies: Lack of essential vitamins like B12 can impair nerve function.
Symptoms and Signs
The telltale signs of neuropathy vary but often include:
- Persistent numbness or tingling in the feet and toes
- Sharp, jabbing, or throbbing pain
- Muscle weakness
- Sensitivity to touch or temperature changes
The Importance of Treatment
Ignoring neuropathy can lead to severe complications, including infections and ulcers. In the worst cases, untreated neuropathy can necessitate amputations due to severe infections and poor wound healing. Hence, timely treatment is not just beneficial but critical.
Treatment Options
Several treatment modalities can help manage neuropathy:
- Medications: Pain relievers, anti-seizure drugs, and antidepressants are commonly prescribed.
- Physical Therapy: Exercises can help improve strength and balance.
- Lifestyle Changes: Quitting smoking, limiting alcohol, and maintaining a healthy diet can make a significant difference.
- Surgical Interventions: In severe cases, surgery might be an option to relieve pressure on nerves.
The Role of Compression Socks
Compression socks can play a pivotal role in both treating and preventing neuropathy. These socks apply gentle pressure to your feet and lower legs, which helps improve blood circulation. Enhanced circulation can reduce swelling, alleviate pain, and promote nerve health.
Technically, compression socks work by exerting graduated pressure, with the most compression at the ankle and gradually decreasing up the leg. This design helps push blood back up towards the heart, reducing the risk of blood pooling in the extremities—a common issue in neuropathy patients.
Conclusion
Peripheral neuropathy affecting the toes and feet is a condition that demands attentive care and proactive treatment. By understanding the causes, recognizing the symptoms, and seeking appropriate treatment—including the use of compression socks—you can manage this condition effectively. If you are experiencing any of these symptoms, consult a healthcare provider to formulate a comprehensive treatment plan tailored to your needs. Your feet are your foundation; take steps to protect them.
For Poor Circulation
Poor Circulation in the Toes, Feet, and Lower Legs:
Poor circulation refers to the inadequate flow of blood to certain parts of the body, particularly the extremities such as the toes, feet, and lower legs. When blood flow diminishes, it deprives these areas of essential oxygen and nutrients, leading to various symptoms and complications.
Prevalence in the UK
In the UK, poor circulation is a prevalent issue, affecting approximately 20% of individuals over the age of 60. It is crucial to understand the seriousness of this condition, as early detection and treatment can prevent severe complications.
Affected Areas
The condition primarily impacts the lower extremities. Your toes, feet, and lower legs are most vulnerable due to their distance from the heart, making it harder for blood to reach these areas efficiently.
Causes and Risk Factors
Several factors contribute to poor circulation, and understanding these can help you identify if you’re at risk:
- Atherosclerosis: The narrowing of arteries due to plaque buildup is a leading cause.
- Diabetes: High blood sugar levels can damage blood vessels.
- Obesity: Excess weight puts additional pressure on the circulatory system.
- Sedentary Lifestyle: Lack of movement leads to poor blood flow.
- Smoking: Nicotine constricts blood vessels, reducing circulation.
- Peripheral Artery Disease (PAD): A condition that narrows the arteries outside of the heart.
Symptoms and Signs
Recognizing the symptoms of poor circulation is vital for timely intervention. Common signs include:
- Coldness in the toes or feet
- Numbness or tingling sensations
- Swelling in the lower legs
- Discoloration of the skin
- Slow-healing sores or ulcers
- Cramping or pain during activities
Importance of Treatment
Ignoring poor circulation can lead to serious complications. Without treatment, you risk developing chronic wounds, infections, and even tissue death, which could necessitate amputation in severe cases. Therefore, addressing the underlying causes is crucial.
Treatment Options
Several treatments can enhance blood flow and alleviate symptoms:
- Lifestyle Changes: Regular exercise, a balanced diet, and quitting smoking can significantly improve circulation.
- Medications: Blood thinners and medications to manage underlying conditions like diabetes and high blood pressure.
- Surgical Interventions: In severe cases, procedures like angioplasty or bypass surgery may be necessary.
The Role of Compression Socks
Compression socks are an effective tool for both treating and preventing poor circulation. These specially designed socks apply gentle pressure to your legs, helping the veins and arteries move blood more efficiently. Here’s how they work:
- Graduated Compression: These socks provide more pressure at the ankle and gradually decrease up the leg, promoting upward blood flow.
- Reduced Swelling: By improving blood flow, they help reduce swelling and discomfort.
- Enhanced Venous Return: Compression socks aid the veins in returning deoxygenated blood to the heart, thus improving overall circulation.
Conclusion
In conclusion, poor circulation in the toes, feet, and lower legs is a concerning condition that requires prompt attention. By understanding the causes, recognizing the symptoms, and exploring the available treatments, you can take proactive steps to manage and prevent this condition. Compression socks, in particular, offer a practical and effective solution for enhancing blood flow and alleviating symptoms. Remember, early intervention is key to maintaining your health and preventing serious complications. If you suspect you have poor circulation, consult with a healthcare professional to explore your treatment options.
For Varicose Veins
Varicose Veins:
Varicose veins—those unsightly, twisted blood vessels that often bulge just beneath the skin—are more than a mere cosmetic concern. This condition can lead to discomfort, pain, and even more serious health complications if left untreated. But what exactly are varicose veins, and how can you manage or prevent them? Let’s delve into this condition with an engaging, informative, and empathetic approach.
What Are Varicose Veins?
Varicose veins are enlarged, swollen veins that often appear as blue or dark purple lines on the legs. These veins become twisted and distorted due to weakened or damaged valves within the veins, which fail to regulate blood flow effectively. This malfunction causes blood to pool in the veins, leading to the characteristic bulging appearance.
How Common Are Varicose Veins?
Varicose veins are surprisingly common. In the UK, approximately 30% of adults are affected by this condition at some point in their lives. This prevalence increases with age, making varicose veins an issue that many will face as they grow older.
What Part of the Body Is Affected?
Varicose veins primarily affect the legs and feet. This is due to the increased pressure in the veins of the lower body when standing or walking. The veins in these parts of the body have to work harder to pump blood back to the heart, which is why they are more prone to becoming varicose.
Causes and Risk Factors
Several factors can increase the risk of developing varicose veins:
- Age: Aging causes wear and tear on the valves in your veins that help regulate blood flow.
- Gender: Women are more likely to develop varicose veins due to hormonal changes during pregnancy, premenstruation, or menopause.
- Family History: Genetics play a role, as varicose veins tend to run in families.
- Obesity: Excess weight increases pressure on your veins, exacerbating the condition.
- Standing or Sitting for Long Periods: Prolonged periods of inactivity can restrict blood flow, leading to varicose veins.
Signs and Symptoms
Recognizing the signs of varicose veins can help in seeking timely treatment:
- Swollen, Bulging Veins: These veins often look twisted and are visible just under the surface of the skin.
- Aching Pain: Legs may feel heavy, achy, or sore, especially after standing or sitting for long periods.
- Swelling: The lower legs, ankles, or feet may become swollen.
- Skin Changes: Discoloration, dryness, or irritation around the affected veins.
Importance of Treatment
Ignoring varicose veins can lead to serious complications. Untreated varicose veins can result in:
- Ulcers: Painful ulcers can form on the skin near varicose veins, particularly around the ankles.
- Blood Clots: The affected veins can become inflamed, leading to blood clots that can be life-threatening.
- Bleeding: Varicose veins close to the skin can burst, causing bleeding.
Treatment Options
There are various treatment options available, depending on the severity of the condition:
- Lifestyle Changes: Regular exercise, weight loss, and elevating the legs can alleviate symptoms.
- Compression Stockings: These are often the first line of treatment. They improve circulation by applying pressure to the legs, reducing swelling and discomfort.
- Sclerotherapy: A solution is injected into the vein, causing it to collapse and fade over time.
- Laser Treatments: High-intensity light is used to close off smaller varicose veins.
- Surgery: In severe cases, surgical options like vein stripping or endoscopic vein surgery may be necessary.
The Role of Compression Socks
Compression socks are a cornerstone in both treating and preventing varicose veins. They apply gradual pressure to your legs, which helps maintain blood flow and reduce swelling. Here’s how they work:
- Encouraging Blood Flow: By compressing the leg tissues, these socks help the veins push blood back up to the heart, combating the pooling of blood.
- Reducing Swelling: Compression socks can help reduce swelling in the legs, ankles, and feet by improving circulation.
- Alleviating Pain: They can relieve the aching and discomfort associated with varicose veins, making daily activities more manageable.
Conclusion
Understanding varicose veins is the first step towards managing this common condition effectively. By recognizing the symptoms and taking proactive measures—such as using compression socks and seeking appropriate medical treatments—you can alleviate discomfort, prevent complications, and improve your quality of life. If you suspect you might have varicose veins, consult a healthcare professional to explore the best treatment options for you.
For Deep vein thrombosis (DVT)
Deep Vein Thrombosis:
Deep vein thrombosis (DVT) is a serious and potentially life-threatening condition that demands immediate medical attention. DVT occurs when a blood clot forms in a deep vein, typically in the lower extremities, such as the legs or thighs. This condition can lead to severe complications, including pulmonary embolism (PE), where a part of the clot breaks off and travels to the lungs, obstructing blood flow and potentially causing sudden death.
What is Deep Vein Thrombosis?
DVT is the formation of a blood clot, or thrombus, in a deep vein. Most commonly, DVT affects veins in the legs. Imagine the veins as highways for your blood, and a clot as a sudden roadblock. This obstruction can impede the return of blood to the heart, leading to swelling, pain, and even tissue damage.
Prevalence and Impact
In the UK, approximately 1 in 1,000 people are affected by DVT each year. This statistic highlights the importance of awareness and prompt medical intervention.
Areas Commonly Affected
DVT primarily impacts the deep veins in the legs, including:
- The calf
- The thigh
- The pelvis
However, blood clots can also form in other parts of the body, such as the arms or abdomen.
Causes and Risk Factors
Several factors can increase the risk of developing DVT:
- Prolonged Immobility: Sitting for extended periods, such as during long flights or car rides, can slow blood flow in the legs.
- Surgery or Trauma: Major surgeries, especially those involving the legs, hips, or abdomen, can damage blood vessels and increase clot risk.
- Genetics: A family history of blood clots can predispose individuals to DVT.
- Medical Conditions: Conditions like cancer, heart disease, and inflammatory bowel disease can increase clotting risk.
- Hormonal Factors: Pregnancy, hormone replacement therapy, and birth control pills can elevate the risk.
- Age and Weight: Older age and obesity are significant risk factors.
Symptoms
Recognizing the signs of DVT is crucial:
- Swelling: Usually in one leg, often accompanied by tenderness or pain.
- Redness and Warmth: Affected areas may become red, warm, and sensitive to touch.
- Cramping: Pain similar to a muscle cramp that typically starts in the calf.
Ignoring these symptoms can lead to severe consequences, such as:
- Pulmonary Embolism (PE): A life-threatening condition where part of the clot breaks off and blocks blood flow to the lungs.
- Post-Thrombotic Syndrome: Long-term pain, swelling, and skin changes in the affected limb.
Importance of Treatment
Immediate treatment is vital to prevent complications. Common treatments include:
- Anticoagulants: Medications that thin the blood to prevent further clotting and to help the body dissolve existing clots.
- Thrombolytics: Drugs that rapidly dissolve clots in life-threatening situations.
- Compression Stockings: Specially designed socks that apply consistent pressure to the legs, promoting blood flow and preventing clot formation.
- Surgical Intervention: Rarely, surgery may be necessary to remove a clot.
Role of Compression Socks
Compression socks are a non-invasive and effective method both for treating and preventing DVT. These socks apply graduated pressure, highest at the ankle and gradually decreasing up the leg. This enhances blood flow and reduces the risk of clot formation. By supporting the veins and improving circulation, compression socks can:
- Reduce Swelling: By promoting fluid return from the legs to the heart.
- Alleviate Pain: By decreasing vein pressure and preventing blood from pooling.
- Prevent Post-Thrombotic Syndrome: By ensuring continuous blood flow and reducing the risk of long-term complications.
Conclusion
Deep vein thrombosis is a condition that should never be taken lightly. By understanding the risk factors, recognizing the symptoms, and seeking prompt medical treatment, you can significantly reduce the risks associated with DVT. Compression socks play a crucial role in managing this condition—ensuring that blood flows efficiently through your veins, preventing further complications, and aiding recovery. Always consult healthcare professionals if you suspect DVT; timely intervention can save your life.
For Chronic Venous Insufficiency
Chronic Venous Insufficiency:
Chronic venous insufficiency is a condition where the veins in your legs are unable to efficiently return blood to your heart. This occurs because the valves in the veins, which usually prevent blood from flowing backward, become damaged or weakened. As a result, blood pools in the legs, leading to various uncomfortable and potentially serious symptoms.
How Common is Chronic Venous Insufficiency?
In the United Kingdom, Chronic venous insufficiency is quite prevalent, affecting approximately 10-15% of men and 20-25% of women. This high incidence underscores the importance of understanding and addressing this condition promptly.
Which Parts of the Body are Affected?
Chronic venous insufficiency primarily affects the veins in the lower extremities—specifically the legs. The malfunctioning of the venous valves leads to blood pooling in the calf muscles and ankles, which are most susceptible to this condition.
Causes and Risk Factors The root causes of Chronic venous insufficiency are multifaceted. Key contributing factors include:
- Heredity: A family history of venous conditions significantly increases your risk.
- Age: The likelihood of developing Chronic venous insufficiency rises with age, as veins and valves naturally weaken over time.
- Gender: Women are more prone to Chronic venous insufficiency, particularly due to hormonal changes during pregnancy and menopause.
- Obesity: Excess weight adds pressure to the veins in your legs, which can exacerbate valve dysfunction.
- Prolonged Standing or Sitting: Occupations that require long periods of standing or sitting can impede blood flow and increase Chronic venous insufficiency risk.
Recognizing the Symptoms
The symptoms of Chronic venous insufficiency can range from mildly discomforting to severely debilitating. Common signs include:
- Swelling: Particularly in the lower legs and ankles.
- Pain or aching: Especially when standing or walking for extended periods.
- Heaviness: A persistent feeling of heaviness in the legs.
- Varicose veins: Enlarged, twisted veins visible under the skin.
- Skin changes: Such as discoloration, itching, or the development of ulcers.
Why Treatment is Crucial
Ignoring Chronic venous insufficiency can lead to serious complications. Untreated, it may result in chronic pain, persistent swelling, skin ulcerations, and even deep vein thrombosis, a condition where blood clots form in the deep veins of the legs. These complications can severely impact your quality of life and may require more intensive medical interventions.
Treatment Options
Effective management of Chronic venous insufficiency involves a combination of lifestyle changes, medical treatments, and, in some cases, surgical procedures. Here are some common treatments:
- Lifestyle Modifications:
- Exercise: Regular physical activity can improve blood flow.
- Weight Management: Maintaining a healthy weight reduces pressure on your veins.
- Elevation: Elevating your legs can help reduce swelling and improve circulation.
- Medical Therapies:
- Medications: Diuretics to reduce swelling or medications to improve blood flow.
- Sclerotherapy: A procedure where a solution is injected into varicose veins, causing them to collapse and fade.
- Surgical Interventions:
- Vein Stripping: Removal of damaged veins.
- Laser Treatment: Using laser energy to close off varicose veins.
The Role of Compression Socks
Compression socks offer several benefits for individuals suffering from CVI, specifically targeting the affected areas in the legs.
Benefits of Compression Socks for CVI
- Reduced Swelling: Compression socks improve blood flow in the legs, which helps to significantly reduce swelling and discomfort in the lower extremities.
- Enhanced Venous Return: By applying gentle pressure, these socks aid the veins in efficiently returning deoxygenated blood to the heart, thereby improving overall circulation and reducing the pooling of blood in the legs.
- Prevention of Varicose Veins: Regular use of compression socks can help prevent the formation of varicose veins, a common symptom of CVI, by maintaining optimal blood flow.
By wearing compression socks, individuals with chronic venous insufficiency can experience substantial relief from the debilitating symptoms that affect the legs, leading to improved overall quality of life.
Understanding and addressing Chronic Venous Insufficiency is crucial to maintaining your leg health and overall well-being. If you suspect you might be suffering from Chronic venous insufficiency, it’s imperative to seek medical advice promptly. By adopting a proactive approach—through lifestyle changes, medical treatments, and the use of compression socks—you can manage this condition effectively and prevent further complications.
Stay informed, take action, and prioritize your vascular health. If you have any concerns or need more personalized advice, don’t hesitate to consult a healthcare professional.
For Lymphedema
Lymphedema:
Lymphedema is a chronic and often debilitating condition that can profoundly impact the quality of life. If you or a loved one are grappling with this condition, understanding its intricacies is essential.
What is Lymphedema?
Lymphedema is a medical condition characterized by the accumulation of lymphatic fluid, leading to swelling, typically in the arms or legs. This occurs due to a compromised lymphatic system, which is responsible for draining excess fluids from tissues. When this drainage system is obstructed or damaged, fluid collects, causing swelling and discomfort.
Prevalence and Affected Areas
In the UK, lymphedema affects approximately 240,000 people, making it a relatively common condition. The swelling primarily occurs in the extremities—arms and legs—but it can also affect other parts of the body, including the chest, head, and neck.
Causes and Risk Factors
Lymphedema can develop due to various underlying causes. Here are some key risk factors:
- Primary Lymphedema: This is a rare, inherited condition caused by developmental abnormalities in the lymphatic system.
- Secondary Lymphedema: More common, it results from damage or blockage of the lymphatic system due to factors such as:
- Surgery: Especially procedures involving lymph node removal.
- Radiation Therapy: Often used in cancer treatments, which can damage the lymphatic system.
- Infections: Certain parasitic infections can cause lymphatic damage.
- Trauma or Injury: Severe injuries can lead to lymphatic blockage.
- Cancer: Tumors can obstruct lymphatic pathways.
Recognizing the Symptoms
Timely identification of lymphedema symptoms is crucial for effective management. Key signs include:
- Swelling: Persistent swelling in the affected limb(s) is the hallmark symptom.
- Heavy Sensation: A feeling of heaviness or tightness in the swollen area.
- Restricted Range of Motion: Swelling can limit movement in the affected limb(s).
- Discomfort or Pain: The swelling can cause varying degrees of pain or discomfort.
- Recurrent Infections: Swollen tissues are prone to infections, such as cellulitis.
Importance of Treatment
Ignoring lymphedema can lead to serious complications. Chronic swelling can cause skin changes, fibrosis (thickening and scarring of tissue), and recurring infections, which can become life-threatening. Moreover, untreated lymphedema can significantly impede daily activities and overall well-being.
Treatment Options
Effective management of lymphedema involves a combination of treatments:
- Manual Lymphatic Drainage (MLD): A specialized massage technique that promotes lymph fluid movement.
- Compression Therapy: Use of compression garments, such as sleeves or socks, to reduce swelling and prevent fluid buildup.
- Exercise: Regular, gentle exercises to enhance lymphatic flow.
- Skincare: Proper skincare to prevent infections and maintain skin health.
- Surgical Interventions: In severe cases, procedures like lymph node transplantation or liposuction might be considered.
The Role of Compression Socks
Compression socks play a pivotal role in both treating and preventing lymphedema. These specially designed garments apply consistent pressure to the affected limbs, helping to:
- Reduce Swelling: By promoting fluid movement and preventing fluid accumulation.
- Improve Circulation: Enhancing blood flow in the legs and feet.
- Prevent Recurrence: Regular use can help maintain reduced swelling and prevent future episodes.
It is important to always consult a doctor before beginning the use of compression socks for lymphedema. Improper use or selection of compression garments can lead to serious complications, such as impaired circulation or skin damage. A healthcare professional can provide guidance on the correct type and compression level needed for individual cases, ensuring safe and effective treatment.
Conclusion
Lymphedema is a manageable condition with the right knowledge and resources. Understanding its causes, symptoms, and treatment options is the first step towards effective management. If you suspect you may have lymphedema, consult a healthcare provider for a comprehensive evaluation and personalized treatment plan. Remember, proactive management can significantly improve your quality of life and prevent complications.
For Edema
Edema:
Edema, also known as swelling, is a condition that affects millions of people worldwide. It is characterized by an excessive accumulation of fluid in the body’s tissues, leading to noticeable swelling. This condition can occur in various parts of the body, including the legs, ankles, feet, hands, and even the face. Let’s delve deeper into what edema is, its causes, symptoms, and the importance of timely treatment.
What is Edema?
Edema refers to the unusual buildup of fluid in the tissues, which can result in swelling. This can happen due to a variety of reasons, ranging from injuries and infections to chronic diseases and certain medications. The fluid typically accumulates in the interstitial spaces, which are the areas between the body’s cells.
Prevalence of Edema
In the UK, edema is relatively common, affecting a significant portion of the population. While exact statistics can vary, it is estimated that around 1 in 10 people may experience some form of edema in their lifetime. The condition is particularly prevalent among individuals with underlying health conditions.
Areas Affected by Edema
Edema can affect almost any part of the body, but it is most commonly observed in the following areas:
- Legs and ankles: This is often due to gravity pulling fluid down into the lower extremities.
- Feet: Swelling in the feet can make it difficult to walk and wear shoes comfortably.
- Hands: This can cause rings to become tight and may limit hand movement.
- Face and eyes: Swelling around the eyes can be particularly noticeable upon waking up.
Causes and Risk Factors
Several factors can contribute to the development of edema. Some of the most common causes include:
- Heart conditions: Congestive heart failure can lead to fluid accumulation in the legs and feet.
- Kidney disease: Impaired kidney function can cause fluid retention throughout the body.
- Liver disease: Conditions like cirrhosis can lead to fluid buildup in the abdomen and legs.
- Pregnancy: Hormonal changes and increased blood volume can cause swelling, particularly in the legs and feet.
- Injury or inflammation: Trauma, infections, or skin conditions can result in localized swelling.
- Medications: Certain drugs, such as those for high blood pressure or diabetes, can cause fluid retention as a side effect.
Symptoms of Edema
The telltale signs of edema include:
- Swelling: Noticeable puffiness in the affected area.
- Stretched or shiny skin: The skin may appear tight and glossy.
- Pitting: Indentation remains for a few seconds after pressing on the swollen area.
- Discomfort or pain: Swelling can be painful, especially if it affects the joints.
- Reduced mobility: Movement can become difficult due to stiffness and swelling.
Importance of Treatment
Treating edema promptly is crucial to avoid potential complications. If left untreated, edema can lead to:
- Skin ulcers: Persistent swelling can cause the skin to break down, leading to sores.
- Infections: Swollen areas are more susceptible to infections like cellulitis.
- Decreased blood circulation: Poor circulation can exacerbate swelling and contribute to other health issues.
- Permanent damage: Chronic edema can cause permanent tissue and skin damage.
Treatment Options
Various treatments are available to manage and alleviate edema:
- Lifestyle changes: Reducing salt intake, elevating the affected limbs, and maintaining a healthy weight can help.
- Medications: Diuretics may be prescribed to help the body expel excess fluid.
- Physical therapy: Exercises can improve circulation and reduce swelling.
- Compression therapy: Compression garments, such as socks and stockings, can provide significant relief.
Role of Compression Socks
Compression socks play a vital role in both treating and preventing edema. These specialized garments apply gentle pressure to the legs, ankles, and feet, which helps:
- Reduce swelling: By promoting blood flow and limiting fluid buildup.
- Improve circulation: Enhancing venous return to the heart, thereby reducing pooling of blood in the lower extremities.
- Prevent blood clots: Compression socks can decrease the risk of deep vein thrombosis (DVT) in individuals prone to edema.
- Provide comfort: Alleviating discomfort and pain associated with swelling.
In summary, edema is a common condition that can have significant impacts on one’s quality of life. Understanding its causes, symptoms, and the importance of timely treatment is essential. Compression socks, among other treatments, offer an effective solution for managing and preventing this condition, ensuring better health and comfort for those affected.
For Leg Fatigue & Discomfort
Leg Fatigue and Discomfort:
Leg fatigue and discomfort can be a daily struggle, affecting your ability to perform routine tasks and diminishing your overall quality of life. Do you often find yourself experiencing persistent tiredness and pain in your legs? You are not alone. This condition is more common than many realize and can have far-reaching impacts if not addressed. Let’s delve deeper into what leg fatigue and discomfort entail, their causes, symptoms, and effective treatments.
What is Leg Fatigue and Discomfort?
Leg fatigue and discomfort refer to a persistent feeling of tiredness, heaviness, and pain in the legs. This sensation is not just about occasional tiredness after a long day. It can be chronic and debilitating, affecting your daily activities and overall well-being.
Prevalence in the UK
In the United Kingdom, leg fatigue and discomfort are surprisingly common. Studies indicate that about 20% of the adult population reports regular leg pain and fatigue. The prevalence increases with age, affecting up to 50% of individuals over the age of 50.
Affected Areas
The condition primarily affects the muscles, veins, and nerves in the legs. The calves, thighs, and feet are particularly susceptible to fatigue and discomfort due to their roles in supporting body weight and facilitating movement.
Causes and Risk Factors
Understanding the root causes of leg fatigue and discomfort is crucial for effective treatment and prevention. Here are some key factors:
- Poor Circulation: Issues like varicose veins can impede blood flow, leading to leg pain and fatigue.
- Prolonged Standing or Sitting: Occupations or lifestyles that require long periods of standing or sitting can strain the leg muscles and veins.
- Age: Aging can weaken the muscles and veins, making older adults more susceptible.
- Obesity: Excess weight puts additional pressure on the legs, exacerbating fatigue and discomfort.
- Pregnancy: Hormonal changes and increased weight during pregnancy can lead to leg pain.
- Medical Conditions: Conditions like diabetes or arthritis can contribute to chronic leg discomfort.
Symptoms to Watch For
Recognizing the symptoms early can prevent further complications. Common tell-tale signs include:
- Persistent tiredness in the legs
- Swelling and inflammation
- Pain and cramping, especially at night
- Heaviness in the legs
- Restless legs syndrome
Importance of Treatment
Ignoring leg fatigue and discomfort can lead to severe consequences. Chronic pain can significantly impair mobility, leading to a sedentary lifestyle, which in turn increases the risk of cardiovascular diseases, obesity, and mental health issues. Early and effective treatment is vital to maintain your quality of life.
Treatment Options
Several treatment methods can alleviate leg fatigue and discomfort, including:
- Exercise: Regular physical activity improves blood flow and strengthens muscles.
- Elevation: Elevating the legs above heart level can reduce swelling and improve circulation.
- Hydration: Keeping well-hydrated helps maintain optimal blood flow.
- Medications: Pain relievers or anti-inflammatory medications can provide temporary relief.
- Physical Therapy: Professional guidance can help target and strengthen affected muscles.
Role of Compression Socks
Compression socks are a highly effective tool for treating and preventing fatigue and discomfort in your legs. These specially designed socks apply gentle pressure, particularly around the calves and ankles, providing several key benefits:
Enhance Circulation: The gentle pressure exerted by compression socks significantly improves blood flow, which can help alleviate symptoms of fatigue and discomfort in the legs. Improved circulation reduces the risk of blood pooling and swelling, providing relief from leg heaviness.
Reduce Swelling: Consistent pressure from compression socks minimizes fluid buildup in the legs. This reduction in swelling can lead to a noticeable decrease in discomfort and fatigue, making daily activities more manageable.
Alleviate Pain: By improving blood flow and reducing swelling, compression socks can significantly diminish pain and discomfort in the legs. This can be particularly beneficial for individuals who spend long periods standing or sitting, as it helps counteract the negative effects of prolonged immobility.
A study published in 2018 investigated the impact of compression socks on leg fatigue and discomfort. The study involved 120 participants who reported chronic fatigue and discomfort in their legs. Participants were divided into two groups: one group wore compression socks daily for a period of 8 weeks, while the control group did not use any form of compression therapy.
Results:
- In the compression sock group, 78% of participants reported a significant reduction in leg pain and discomfort.
- There was a 65% decrease in reported leg swelling.
- The control group showed no significant changes in symptoms.
The study concluded that compression socks are an effective intervention for reducing fatigue, pain, and swelling in the legs, thereby improving the overall quality of life for individuals experiencing these symptoms.
By incorporating compression socks into your routine, you can experience substantial relief from the fatigue and discomfort affecting your legs.
Conclusion
Leg fatigue and discomfort are more than just a minor inconvenience; they are a serious condition that can affect your overall health and well-being. Understanding the causes, recognizing the symptoms, and pursuing effective treatment options, including the use of compression socks, can make a significant difference. Don’t ignore the early signs—take proactive steps to manage and prevent this condition, ensuring a healthier, more active lifestyle.
For Sports & Exercise
Sports and Exercise:
When it comes to running, exercising, or playing sports, our legs and feet endure significant stress. It’s easy to overlook the importance of proper support, but this can lead to severe consequences. Without compression socks, athletes risk developing issues such as muscle fatigue, swelling, and even more severe conditions like deep vein thrombosis (DVT)—a type of blood clot. According to the NHS, around 1 in 1,000 people in the UK are affected by DVT annually. This statistic underscores the importance of preventative measures, such as wearing compression socks.
The Solution: Compression Socks
Compression socks offer a specific form of support, applying gentle pressure to your legs and feet. This pressure helps your blood vessels work more efficiently. But how exactly do they work?
Compression socks are designed to provide graduated compression, meaning they are tighter at the ankle and gradually looser up the leg. This design helps push blood back towards the heart, combating the effects of gravity. When you run or exercise, your muscles need more oxygen-rich blood. Compression socks enhance circulation, delivering this vital resource more efficiently to your muscles.
The Benefits and How They Help
Wearing compression socks can significantly enhance your athletic performance and overall comfort. Here’s how:
- Enhanced Performance: By improving blood circulation, compression socks ensure your muscles get the oxygen they need to perform at their best. This results in better endurance and less fatigue during prolonged activities.
- Injury Prevention: The added support to your feet and ankles can prevent common injuries like sprains and strains. Furthermore, the improved circulation reduces muscle fatigue, which is a common cause of injuries.
- Faster Recovery: After a workout, your muscles need time to repair and recover. Compression socks help speed up this process by maintaining efficient blood flow, reducing muscle soreness, and minimizing swelling.
- Overall Comfort: Beyond the performance benefits, compression socks simply make your legs and feet feel better. They reduce the heaviness and tiredness often felt after long runs or intensive workouts. This can make a significant difference in your overall exercise experience.
In summary, compression socks are a small investment with substantial payoffs. They not only enhance your performance and comfort but also protect against potentially severe health issues. So next time you lace up for a run, a workout, or a game, consider slipping on a pair of compression socks.
For Long-Distance Travel
Long-Distance Travel:
Long-distance travel, whether by flight or car, can be more than just uncomfortable—it can be dangerous. Extended periods of immobility can increase the risk of developing serious health issues, particularly for those with pre-existing conditions. Compression socks are a simple but effective solution to mitigate these risks, offering crucial support and promoting better circulation in your legs and feet. But let’s dive deeper into why these seemingly ordinary socks are so vital.
The Life-Threatening Risks
When you’re seated for long durations, your blood flow slows down, especially in the lower extremities. This sluggish circulation can lead to Deep Vein Thrombosis (DVT), a condition where blood clots form in veins deep within the body, often in the legs. According to the UK National Health Service (NHS), around 25,000 hospital patients die from preventable blood clots each year. This figure underscores the gravity of the situation.
People with conditions like varicose veins, obesity, or a history of blood clots are at an even higher risk. The consequences of ignoring this risk can be severe, even fatal. A blood clot could dislodge and travel to the lungs, causing a pulmonary embolism—a life-threatening condition.
Don’t Solely Rely on Compression Socks
While compression socks are highly beneficial, they should not be your only measure against these risks. It’s equally important to keep moving your legs and feet when seated for extended periods. Simple actions like flexing your ankles, stretching your calves, or taking short walks can significantly reduce the risk of blood clots.
How Compression Socks Work
Compression socks apply gentle pressure to your legs, promoting blood flow back to your heart. This graduated compression is tighter at the ankle and gradually decreases up the leg, which helps prevent blood from pooling in the veins. By encouraging better circulation, these socks reduce swelling and alleviate discomfort.
The Benefits of Wearing Compression Socks
Wearing compression socks can profoundly impact various parts of your body. They help prevent swelling in the ankles and feet, alleviate leg pain, and reduce the risk of developing varicose veins. Improved circulation also means less fatigue and a lower likelihood of muscle cramps. For those who suffer from chronic venous insufficiency (a condition where the veins fail to return blood efficiently to the heart), compression socks can be a lifesaver.
Moreover, the benefits extend beyond just physical health. Knowing that you’re taking proactive steps to safeguard your well-being reduces anxiety and stress, making your journey more pleasant. Enjoy your trip with peace of mind!
Practical Tips for Long-Distance Travel
While compression socks are highly effective, they work best when combined with other preventive measures. Stay hydrated by drinking plenty of water—this helps maintain your blood’s consistency, reducing the risk of clots. Avoid crossing your legs, as this can further impede blood flow. If you’re flying, walk around the cabin periodically. For car trips, plan stops to stretch your legs.
Consider the small exercises you can do while seated. Point your toes and then flex them back towards you. Rotate your ankles in circles. These minor movements can significantly improve blood flow.
Conclusion
In essence, compression socks are an invaluable tool for long-distance travel. They offer targeted support, promote circulation, and reduce the risk of potentially life-threatening conditions like DVT. But remember, they are just one piece of the puzzle. Stay active, hydrated, and mindful of your body’s needs.
Taking these steps doesn’t just protect your health—it enhances your travel experience. So next time you embark on a long journey, don’t just pack your essentials; include a good pair of compression socks. Safe travels!
For Hypotension
Postural Hypotension:
Are you frequently feeling lightheaded or dizzy when you stand up? This could be a sign of a condition known as postural hypotension, also referred to as orthostatic hypotension. Let’s delve deeper into what this condition entails, how it affects your body, and the steps you can take to manage or even prevent it.
What is Postural Hypotension?
Postural hypotension is a sudden drop in blood pressure that occurs when you move from sitting or lying down to a standing position. This drop causes a temporary decrease in blood flow to the brain, which often results in dizziness, lightheadedness, or even fainting. It’s more than just a minor inconvenience; it can significantly affect your quality of life and, if left untreated, lead to more serious health issues.
How Common is Postural Hypotension?
In the UK, postural hypotension is relatively common, especially among older adults. Studies indicate that it affects about 20% of people over the age of 65. However, it can also occur in younger individuals due to various underlying health conditions or lifestyle factors.
Affected Body Parts and Causes
Postural hypotension primarily affects the cardiovascular and nervous systems. The heart, blood vessels, and brain are most impacted, as they work together to regulate blood pressure and ensure adequate blood flow when you change positions.
Several factors contribute to postural hypotension:
- Dehydration: When your body lacks sufficient fluids, your blood volume decreases, leading to lower blood pressure.
- Heart conditions: Ailments such as heart failure, heart attack, or arrhythmias can impair the heart’s ability to pump blood effectively.
- Endocrine disorders: Conditions like diabetes or adrenal insufficiency can affect the body’s blood pressure regulation.
- Medications: Certain drugs, including those for high blood pressure, can cause postural hypotension as a side effect.
- Neurological conditions: Diseases such as Parkinson’s or multiple system atrophy can impact the nervous system’s ability to control blood pressure.
Symptoms and the Importance of Treatment
The hallmark symptoms of postural hypotension include dizziness, lightheadedness, blurred vision, weakness, and, in severe cases, fainting upon standing up. These symptoms can be more than just uncomfortable; they can increase your risk of falls and related injuries, which can be particularly dangerous for older adults.
Ignoring postural hypotension can lead to severe complications, including chronic fatigue, cognitive impairment, and even an increased risk of stroke. Therefore, timely and effective treatment is crucial.
Treatment Options
Several treatment strategies can help manage postural hypotension:
- Lifestyle changes: Increasing fluid and salt intake, eating smaller meals, and avoiding alcohol can help maintain blood pressure.
- Physical maneuvers: Techniques such as crossing your legs while standing or tensing your leg muscles can improve blood flow.
- Medications: Drugs like fludrocortisone or midodrine may be prescribed to help raise blood pressure.
- Compression garments: Wearing compression stockings or abdominal binders can prevent blood from pooling in your legs and improve circulation.
The Role of Compression Socks
Compression socks are a particularly effective tool in managing postural hypotension by applying graduated pressure to the legs, which supports the veins and enhances blood return to the heart. This helps maintain blood flow, reduces the pooling of blood in the lower extremities, and ensures a steadier blood flow when moving to a standing position. As a result, the improved circulation alleviates symptoms such as dizziness and lightheadedness, reducing the likelihood of fainting and helping to prevent falls.
It is crucial to consult a doctor before wearing compression socks for postural hypotension. A medical professional can provide personalized advice and ensure that the compression level is appropriate for your condition. Improper use of compression socks can lead to serious risks such as impaired circulation, skin damage, or worsening of symptoms. Therefore, a doctor’s guidance is essential to avoid potential complications and ensure the safe and effective use of compression socks.
Conclusion
Understanding and managing postural hypotension is essential to maintaining a high quality of life. By recognizing the symptoms and underlying causes, you can take proactive steps to address this condition. Whether through lifestyle changes, medications, or the use of compression socks, effective management is within reach. Remember, your health and well-being are paramount, and taking the necessary steps to manage postural hypotension can make a significant difference.
For Diabetic Foot Complications
Diabetic Foot Complications:
Diabetic foot complications arise as a result of prolonged high blood sugar levels that damage nerves and blood vessels in the feet. This can lead to a range of issues from minor cuts that don’t heal properly to severe infections and, in the worst cases, amputations. Imagine not feeling a pebble in your shoe until it creates a sore that gets infected; this is a reality for many living with diabetes.
How Common is it?
In the UK, it’s estimated that around 10% of people with diabetes will experience a foot ulcer at some point in their lives. This statistic underscores the importance of being vigilant, paying close attention to symptoms, and taking preventive measures.
Parts of the Body Affected
Primarily, diabetic foot complications affect the feet, but the implications can extend beyond. Poor blood flow and nerve damage (neuropathy) can lead to issues in the legs and, in severe cases, impact overall mobility and quality of life.
Who is at Risk?
Certain factors elevate the risk of developing diabetic foot complications:
- Long-term Diabetes: The longer you have diabetes, the greater the risk of complications.
- Poor Blood Sugar Control: Consistently high blood sugar levels increase the risk of damage to nerves and blood vessels.
- Smoking: Smoking impedes blood circulation, exacerbating the risk of foot problems.
- Existing Foot Deformities: Conditions such as bunions or hammertoes can increase the risk of ulcers.
Common Signs and Symptoms
Recognizing the symptoms early is crucial. Look out for:
- Numbness or tingling in the feet: A sign of nerve damage.
- Foot ulcers or sores that do not heal: Indicating poor blood circulation.
- Swelling and redness: Potential signs of an underlying infection.
- Persistent pain: Particularly if it worsens over time.
The Importance of Treatment
Ignoring diabetic foot complications can lead to severe consequences, including infections, gangrene, and ultimately, amputation. Timely treatment is essential to manage symptoms and prevent these dire outcomes.
Treatment Options
Treatment for diabetic foot complications can vary based on the severity:
- Blood Sugar Management: Keeping blood sugar levels within a target range is fundamental.
- Wound Care: Proper cleaning and dressing of wounds are crucial.
- Antibiotics: To combat infections.
- Surgery: In severe cases, surgery may be necessary to remove dead tissue or correct deformities.
The Role of Compression Socks
Compression socks can be a valuable tool in both treating and preventing complications associated with diabetic feet. These specially designed socks apply gentle pressure to the legs and feet, enhancing blood circulation and addressing several key issues that affect individuals with diabetes.
Improve Blood Flow
Diabetic foot complications often arise due to poor blood circulation. Compression socks enhance circulation in the feet and lower legs, which is crucial for those with diabetes. Improved blood flow can facilitate better nutrient and oxygen delivery to the tissues, promoting healing and reducing the risk of ulcers.
Reduce Swelling
Edema, or fluid buildup, is a common issue in diabetic feet. Compression socks help manage this condition by applying pressure that prevents fluid accumulation, thereby reducing swelling. This can lead to increased comfort and mobility for individuals with diabetes.
Minimize Risk of Blood Clots
Diabetic individuals are at a higher risk of developing deep vein thrombosis (DVT) due to impaired circulation. By promoting better blood flow, compression socks can reduce the risk of blood clots forming in the veins of the lower legs.
By improving blood flow, reducing swelling, and minimizing the risk of blood clots, compression socks can play a crucial role in managing diabetic foot complications. This makes them an essential component in the comprehensive care and management of diabetic patients.
Conclusion
Understanding and managing diabetic foot complications involves a proactive approach and a keen awareness of potential risks and symptoms. By maintaining good blood sugar control, addressing symptoms early, and utilizing tools such as compression socks, you can significantly improve your foot health and overall well-being. Remember, prevention and prompt treatment are your best defenses against the serious consequences of diabetic foot complications. Stay informed, stay vigilant, and take proactive steps to protect your health.
For Spider Veins
Spider Veins:
Have you ever noticed those small, web-like clusters of red, blue, or purple veins just beneath your skin? These are commonly known as spider veins, a condition that affects many individuals. Let’s delve into what exactly spider veins are, the causes, risk factors, and most importantly, how you can manage and potentially prevent this condition.
What Are Spider Veins?
Spider veins, medically termed telangiectasias, are small, dilated blood vessels that appear close to the surface of the skin. They often form thin, branch-like patterns and can resemble a spider’s web—hence the name. While they can develop anywhere on the body, they are most commonly seen on the legs and face.
How Common Are Spider Veins?
Spider veins are quite prevalent. In the UK, it’s estimated that approximately 30% of women and 25% of men experience this condition at some point in their lives. This indicates a significant portion of the population may grapple with the aesthetic and sometimes discomforting aspects of spider veins.
Areas Affected by Spider Veins
While spider veins can appear almost anywhere, they predominantly affect the legs due to the increased pressure in the veins of the lower body from standing and walking. They can also appear on the face, often around the nose, cheeks, and chin.
Causes and Risk Factors
Understanding the causes of spider veins can help in managing and preventing them. Here are some key factors:
- Genetics: If your family members have had spider veins, you are more likely to develop them.
- Age: As you get older, the valves in your veins may weaken, leading to spider veins.
- Gender: Women are more prone to spider veins, partly due to hormonal changes during pregnancy, menopause, and the use of birth control pills.
- Prolonged Standing or Sitting: Occupations that require long periods of standing or sitting can increase the risk due to prolonged pressure on the veins.
- Obesity: Excess weight puts additional pressure on your veins.
- Sun Exposure: Excessive sun exposure, especially for fair-skinned individuals, can cause spider veins on the face.
Symptoms of Spider Veins
While spider veins are usually painless, they can sometimes cause discomfort. Common symptoms include:
- Visible red, blue, or purple veins
- Itching around the affected area
- A feeling of heaviness or aching in the legs
- Swelling in the legs
Importance of Treatment
Ignoring spider veins can lead to more serious complications, such as:
- Ulcers: Open sores can form, especially near the ankles.
- Bleeding: The veins close to the skin can rupture and bleed.
- Blood Clots: In severe cases, the veins can lead to blood clots.
Early treatment can prevent these complications and improve your overall vein health.
Treatment Options
Several treatment options are available for spider veins. These include:
- Sclerotherapy: This involves injecting a solution into the vein, causing it to collapse and fade.
- Laser Treatments: Focused laser light destroys the vein, which is then absorbed by the body.
- Vein Ligation and Stripping: Surgical removal of the affected veins for more severe cases.
- Lifestyle Changes: Regular exercise, maintaining a healthy weight, and avoiding prolonged periods of standing or sitting.
The Role of Compression Socks
Compression socks are a valuable tool in both the treatment and prevention of spider veins. Here’s how they help:
- Improving Blood Flow: Compression socks apply gentle pressure to your legs, aiding blood flow back to the heart and reducing the pressure in your veins.
- Reducing Swelling: By controlling swelling, compression socks can alleviate the discomfort associated with spider veins.
- Preventing New Veins: For those prone to spider veins, wearing compression socks can help prevent new veins from forming.
Specifically, compression socks are beneficial for the legs, where the effects of gravity and prolonged standing are most pronounced. By providing consistent pressure, they support vein health and reduce the risk of complications.
Conclusion
Spider veins are a common condition that many people face, but with the right knowledge and tools, they can be managed effectively. Understanding the causes, recognizing the symptoms, and seeking early treatment are critical steps. Moreover, incorporating compression socks into your daily routine can play a significant role in both treatment and prevention. If you are experiencing spider veins, don’t hesitate to consult a healthcare professional for advice and appropriate treatment options. Your vein health is an essential part of your overall well-being.
For Phlebitis
Phlebitis:
Phlebitis is a condition characterized by the inflammation of a vein, usually in the legs. It can be a painful and concerning issue, but understanding it thoroughly is the first step to managing and preventing it. Let’s delve into the details that will help you comprehend this condition, recognize its symptoms, and explore the treatment options available.
What Exactly Is Phlebitis?
Phlebitis, derived from the Greek word “phleps” meaning vein, specifically refers to the inflammation of a vein. When a vein becomes inflamed, it can cause significant discomfort and may lead to complications if not addressed promptly. This condition can either be superficial (affecting veins close to the skin’s surface) or deep (impacting deeper veins within the body).
How Common Is Phlebitis?
In the UK, superficial phlebitis is a relatively common condition, often affecting individuals over the age of 60. Statistics show that about 3-11% of people will experience superficial phlebitis at some point in their lives. Deep vein thrombophlebitis (DVT), a more severe form, affects approximately 1 in 1,000 people annually.
What Part of Your Body Does Phlebitis Affect?
Phlebitis most commonly affects the legs, where blood flow can be more easily compromised due to gravity and the body’s natural venous system. It can also affect veins in other parts of the body, but this is less common.
What Causes Phlebitis?
Several factors can cause phlebitis, and understanding these can help in both treatment and prevention. Here are four primary causes:
- Injury to a Vein: Trauma or injury to a vein can trigger inflammation.
- Prolonged Inactivity: Extended periods of inactivity, such as long flights or bed rest, can increase the risk.
- Medical Conditions: Conditions like varicose veins or blood-clotting disorders can predispose individuals to phlebitis.
- Intravenous Catheters: Medical procedures involving IV catheters can irritate the veins, leading to inflammation.
Who Is More at Risk?
Certain individuals have a higher risk of developing phlebitis. These include:
- Older Adults: Age-related changes in the veins can make inflammation more likely.
- Pregnant Women: Pregnancy increases blood volume and puts extra pressure on the veins.
- Individuals with Varicose Veins: These veins are already compromised, making them more susceptible.
- Sedentary Individuals: Lack of movement can impede blood flow, increasing risk.
Common Signs and Symptoms
Recognizing the signs and symptoms of phlebitis is crucial for timely treatment. Common indicators include:
- Pain and Tenderness: The affected area may be painful to touch.
- Redness and Warmth: Inflammation often causes redness and warmth in the skin over the vein.
- Swelling: The area around the affected vein may swell.
- Hardening of the Vein: The vein may feel hard or cord-like under the skin.
Why Is Treatment Important?
Ignoring phlebitis can lead to severe complications such as:
- Deep Vein Thrombosis (DVT): A blood clot in a deep vein can travel to the lungs, causing a potentially life-threatening pulmonary embolism.
- Infection: Inflammation can lead to an infection, exacerbating symptoms and complicating treatment.
- Chronic Venous Insufficiency: Long-term damage to the veins can impair blood flow, leading to chronic issues.
Treatment Options for Phlebitis
Treating phlebitis involves a combination of medical intervention and self-care. Here are the primary treatment options:
- Medications: Anti-inflammatory drugs and pain relievers can reduce discomfort and swelling.
- Compression Therapy: Compression socks or stockings can improve blood flow and reduce swelling.
- Elevation and Rest: Keeping the affected limb elevated can alleviate symptoms.
- Warm Compresses: Applying warm compresses can soothe pain and reduce inflammation.
- Antibiotics: If an infection is present, antibiotics may be necessary.
The Role of Compression Socks
Compression socks are a key component in both the treatment and prevention of phlebitis. These specially designed socks apply graduated pressure to the legs, which helps:
- Improve Blood Circulation: By applying pressure, compression socks enhance venous return, reducing the risk of blood pooling in the veins.
- Reduce Swelling: Compression helps prevent fluid accumulation, alleviating swelling and discomfort.
- Prevent Blood Clots: Improved circulation reduces the risk of clot formation, a critical factor in preventing complications from phlebitis.
- Support Vein Health: Consistent use of compression socks strengthens vein walls and supports overall vascular health.
In conclusion, understanding phlebitis is the first step toward effective management and prevention. Recognizing the symptoms, knowing the risk factors, and adhering to recommended treatments can significantly improve your quality of life. Remember, early intervention is crucial, and using tools like compression socks can make a substantial difference in both treating and preventing this condition. Take proactive steps today to ensure healthier veins and a more comfortable tomorrow.
For Leg injury Recovery
Recovery from Leg Injuries:
Leg injuries affect thousands of individuals in the UK each year, with the NHS reporting over 200,000 cases annually. It’s not just the immediate pain or inconvenience that poses a risk—there’s a host of complications that can arise if these injuries aren’t managed effectively. For instance, complications such as deep vein thrombosis (DVT) can develop, especially if you have underlying conditions like diabetes or cardiovascular disease. DVT involves the formation of blood clots in deep veins, often in the legs. These clots can travel to the lungs, causing a potentially fatal pulmonary embolism. Scary, right? But here’s where compression socks come to the rescue.
Benefits of Compression Socks for Recovery
Compression socks can be highly beneficial for individuals recovering from a leg injury. By enhancing blood circulation in the injured leg and surrounding areas, these socks not only reduce swelling and alleviate pain but also play a crucial role in accelerating the natural healing process of damaged cells. Improved circulation ensures that oxygen and essential nutrients are delivered more efficiently to the injury site, which speeds up tissue repair and regeneration. This expedited recovery allows individuals to resume daily activities more swiftly and helps in preventing serious complications such as deep vein thrombosis (DVT) and chronic venous insufficiency (CVI) that can arise due to prolonged immobility or poor circulation. Additionally, compression socks can aid in preventing the formation of varicose veins, which are a common consequence of compromised blood flow in the legs.
Important Considerations
Despite the clear benefits, it is crucial to consult a healthcare professional before incorporating compression socks into your recovery regimen. Incorrect usage can lead to adverse effects such as impaired circulation, skin irritation, or even worsening of the condition. More seriously, improper use of compression socks can result in the development of blood clots, which are potentially life-threatening if they travel to vital organs such as the lungs, causing a pulmonary embolism. Medical guidance ensures that the compression level is appropriate for your specific condition and that the socks are used correctly, thereby maximizing benefits and minimizing risks.
Conclusion
In conclusion, the use of compression socks in managing leg injuries is not merely advisable—it’s essential. By incorporating compression socks into your recovery regimen and following medical advice, you can promote faster and more effective healing, while significantly mitigating the risks of severe venous complications. You’re not just treating an injury; you’re safeguarding your overall health and well-being.
For Standing For long Periods
Prolonged Standing:
Standing for long periods can take a significant toll on your legs and feet. Let’s delve into why compression socks are an essential ally for those who spend extensive hours on their feet and what makes them so crucial in maintaining your overall health.
Prolonged standing can lead to various health issues, including varicose veins (enlarged, twisted veins), edema (swelling caused by fluid retention), and chronic venous insufficiency (poor blood flow in the veins). According to a study by the Health and Safety Executive (HSE) in the UK, approximately 30% of workers who stand for prolonged periods suffer from leg pain and discomfort annually. This is a significant number, highlighting the need for effective preventive measures.
How Compression Socks Can Help
Compression socks work by providing graduated compression, meaning the pressure is highest at the ankle and gradually decreases up the leg. This design counteracts the effects of gravity, aiding in the efficient return of blood to the heart. By improving blood circulation, compression socks reduce the risk of developing varicose veins and edema. They also help alleviate symptoms of chronic venous insufficiency by preventing blood from pooling in the veins.
Supporting Evidence
A 2018 study published in the Journal of Occupational Health evaluated the efficacy of compression socks in workers who stand for extended periods. The study involved 150 participants from various industries, including healthcare and retail, who were randomly assigned to either a control group or a group wearing compression socks. Over a period of six months, the study measured instances of leg pain, swelling, and varicose vein formation.
Results and Analysis
- Leg Pain: The group wearing compression socks reported a 40% reduction in leg pain compared to the control group.
- Swelling (Edema): There was a 35% decrease in the incidence of edema among those wearing compression socks.
- Varicose Veins: The formation of new varicose veins was reduced by 25% in the compression sock group.
These figures underscore the effectiveness of compression socks in mitigating the adverse effects of prolonged standing. The study provides robust evidence that compression socks are a valuable preventive measure for those who must stand for extended periods, significantly improving comfort and vascular health.
Conclusion
In summary, compression socks are a vital tool for anyone who stands for extended periods. They provide essential support to your legs and feet, preventing a range of health issues and improving your overall well-being. Ignoring the need for compression can lead to severe consequences, but embracing this simple yet effective solution can transform your daily experience, making prolonged standing more manageable and less detrimental to your health.
By understanding the importance of compression socks and the risks of prolonged standing, you’re better equipped to make informed decisions about your health. Remember, taking care of your legs today can prevent a host of problems tomorrow. So, why wait? Invest in a pair of compression socks and experience the benefits for yourself!
For Sitting For long Periods
Prolonged Sitting
Sitting for extended periods, whether at a desk, during a long-haul flight, or while driving, can be more harmful than you might think. While it may seem like a harmless activity, prolonged sitting can lead to a host of health problems that could significantly affect your quality of life. One simple yet effective solution to mitigate these risks is wearing compression socks.
Understanding the Risks
When you sit for long periods, blood flow in your legs can become sluggish. This can lead to conditions such as deep vein thrombosis (DVT), where blood clots form in the deep veins of your legs. According to the NHS, there are approximately 25,000 cases of DVT in the UK each year. If a clot breaks loose, it can travel to your lungs, causing a potentially fatal pulmonary embolism. Additionally, sitting for long durations can result in varicose veins, swollen ankles, and general leg discomfort.
Imagine this: you’re at your desk, engrossed in work, but beneath the surface, the blood in your legs is pooling. Over time, this can lead to chronic venous insufficiency (CVI), a condition where your veins can’t efficiently return blood to your heart. This can cause symptoms like pain, swelling, and skin changes.
How Compression Socks Work
So, how do compression socks help? These specially designed socks apply gentle pressure to your legs and feet, compressing the surface veins, arteries, and muscles. This pressure forces circulating blood through narrower channels, which helps the valves in your veins work more efficiently. Consequently, blood flows more smoothly, reducing the risk of clotting and improving overall circulation.
The Benefits of Compression Socks
Wearing compression socks offers a multitude of benefits. Firstly, they provide essential support to your calf muscles and lower legs, promoting better blood flow. This can alleviate the discomfort and swelling often experienced after long periods of inactivity. For those who suffer from chronic conditions like CVI, compression socks can offer significant relief by aiding in the proper circulation of blood back to the heart.
Moreover, these socks are not just for those with existing health conditions. Even if you’re healthy, compression socks can serve as a preventive measure. They can keep your legs feeling fresh and energized, reducing the feeling of heaviness that often accompanies prolonged sitting. Enhanced circulation means more oxygen and nutrients are delivered to your muscles, which can help in quicker recovery from physical activity.
The Bigger Picture
It’s essential to consider the broader implications of not taking preventive measures like wearing compression socks. Ignoring the risks associated with prolonged sitting can lead to more severe health issues down the line, requiring more invasive treatments and interventions. The old adage “an ounce of prevention is worth a pound of cure” couldn’t be more applicable here.
In summary, the importance of wearing compression socks during long periods of sitting cannot be overstated. They offer a simple, effective way to promote better circulation, reduce the risk of serious health issues, and enhance overall leg comfort. By taking this small step, you’re investing in your long-term health and well-being.
For Muscle soreness
Muscle Soreness:
Muscle soreness, often referred to as delayed onset muscle soreness (DOMS), typically emerges 12 to 24 hours after strenuous activity and can last up to 72 hours. It is characterized by tenderness, stiffness, and sometimes swelling in the affected muscles. Although often a normal response to physical activity, it can be quite uncomfortable and impact daily activities.
Prevalence in the UK
Muscle soreness is incredibly common. In the UK, studies show that about 80% of individuals who engage in regular physical activity have experienced muscle soreness at some point. This condition does not discriminate by age or fitness level, affecting both seasoned athletes and those new to exercise.
Affected Areas
While muscle soreness can affect any part of the body, the legs and feet are particularly vulnerable. This is due to their constant use in activities such as walking, running, and standing. The muscles most commonly affected include the quadriceps, hamstrings, calves, and the muscles in the feet.
Causes and Risk Factors
Muscle soreness is primarily caused by microscopic damage to muscle fibers that occur during physical exertion. This damage triggers an inflammatory response, leading to pain and stiffness. Several factors can increase the risk of developing muscle soreness:
- Sudden Increase in Activity: Engaging in an exercise routine that is more intense or longer in duration than you’re accustomed to.
- Eccentric Exercises: Movements that lengthen the muscle under tension, such as downhill running or lowering weights.
- Lack of Conditioning: Poor physical conditioning and flexibility can make muscles more susceptible to damage.
- Age: Older adults are more prone to muscle soreness due to natural muscle degeneration.
- Genetics: Some individuals may be more genetically predisposed to muscle soreness.
Symptoms and Importance of Treatment
Common symptoms include muscle stiffness, swelling, tenderness, reduced range of motion, and temporary loss of muscle strength. Ignoring these symptoms can lead to more serious complications such as chronic pain, muscle imbalances, and even long-term injury. Therefore, timely and effective treatment is essential.
Risks of Ignoring Muscle Soreness
If left untreated, muscle soreness can escalate and result in severe conditions like stress fractures, muscle strains, and ligament injuries. Chronic muscle imbalance can also develop, leading to poor posture and gait, which can further complicate mobility and overall physical health.
Treatment Options
Treating muscle soreness involves a combination of rest, hydration, and targeted therapies. Some effective treatments include:
- Rest and Recovery: Allowing the muscles to recover by limiting activity.
- Ice Therapy: Applying ice packs to reduce inflammation and numb the affected area.
- Massage: Promoting blood flow and reducing tension through therapeutic massage.
- Hydration: Drinking plenty of water to flush out toxins and support muscle repair.
- Over-the-Counter Medications: Using pain relievers like ibuprofen for temporary relief.
Role of Compression Socks
Compression socks can play a crucial role in both treating and preventing muscle soreness. These specialized garments apply graduated pressure to your legs, promoting blood flow and reducing the buildup of lactic acid. Here’s how they work:
- Enhanced Circulation: Compression socks help to improve venous return, which means blood flows more efficiently back to the heart. This reduces muscle fatigue and speeds up recovery.
- Reduced Swelling: By minimizing fluid buildup in the tissues, compression socks can significantly reduce swelling and discomfort.
- Support and Stability: These socks provide extra support to the muscles and joints, decreasing the risk of strains and injuries.
- Prevention of DOMS: Regular use of compression socks can help in reducing the severity of muscle soreness, allowing you to maintain your fitness routine with minimal disruption.
Conclusion
Muscle soreness in the legs and feet is a widespread condition that can affect anyone. Understanding its causes, symptoms, and the importance of timely treatment can help manage and prevent it effectively. Incorporating treatments such as rest, hydration, and the use of compression socks can significantly alleviate symptoms and promote faster recovery.
For Recovering From Surgery
Post-Surgery Recovery:
Recovering from surgery is a critical period that demands attention and care. Complications during this phase can be life-threatening, yet many are preventable with the right knowledge and measures. This guide aims to provide an engaging, authoritative, and concerned overview of post-surgery recovery, focusing on avoiding possible complications and ensuring a smooth healing process.
What is Post-Surgery Recovery?
Post-surgery recovery refers to the period following a surgical procedure when the body heals and regains strength. This phase is crucial as it determines the success of the surgery and the patient’s overall health. It involves wound healing, pain management, and regaining normal function. However, this period is not without risks. Complications can arise, potentially leading to severe health issues if not properly managed.
How Common Are Post-Surgical Complications?
In the UK, post-surgical complications are not uncommon. Approximately 30% of patients undergoing major surgeries experience some form of complication. These can range from minor issues, such as infections, to more severe problems like deep vein thrombosis (DVT) or pulmonary embolism (PE). Understanding the risks and taking preventive measures is vital to avoid these complications.
Parts of the Body Affected
Post-surgical complications can affect various parts of the body, depending on the type of surgery performed. Commonly affected areas include:
- Surgical Wound: Risk of infection and poor healing.
- Lungs: Risk of pneumonia, especially after abdominal or thoracic surgery.
- Legs: Risk of DVT and PE, particularly after orthopedic surgeries.
- Heart: Risk of cardiac events, especially in patients with preexisting heart conditions.
Causes and Risk Factors
Several factors contribute to post-surgical complications. Understanding these can help identify those at higher risk and implement preventive strategies. Key factors include:
- Type of Surgery: Major surgeries have a higher risk of complications.
- Age: Older adults are more susceptible to complications due to a weaker immune system.
- Preexisting Conditions: Conditions like diabetes, obesity, and heart disease increase the risk.
- Lifestyle Factors: Smoking, poor nutrition, and lack of physical activity can impair recovery.
- Immune System Function: A weakened immune system can hinder healing and increase infection risk.
Common Signs and Symptoms
Recognizing the signs and symptoms of post-surgical complications is essential for timely intervention. Common indicators include:
- Fever: May indicate infection.
- Excessive Pain: Could signify wound issues or internal complications.
- Swelling and Redness: Often associated with infections or DVT.
- Shortness of Breath: Can be a sign of PE or pneumonia.
- Unusual Discharge from Wounds: Indicates possible infection.
Importance of Treatment and Risks of Ignoring the Problem
Prompt treatment of post-surgical complications is crucial. Ignoring these issues can lead to severe consequences, such as:
- Infections: Can spread, leading to sepsis, a life-threatening condition.
- DVT and PE: Can cause significant morbidity and even mortality.
- Delayed Healing: Can prolong recovery time and affect the overall outcome of the surgery.
- Chronic Pain: Untreated complications can result in persistent pain and discomfort.
Treatment Options
Treatment for post-surgical complications varies based on the specific issue but generally includes:
- Antibiotics: For infections.
- Anticoagulants: To prevent or treat DVT and PE.
- Pain Management: Medications and therapies to control pain.
- Physical Therapy: To regain strength and mobility.
- Wound Care: Specialized dressings and care procedures to promote healing.
The Role of Compression Socks
Compression socks play a significant role in both treating and preventing post-surgical complications, particularly those related to the legs, such as DVT. These socks apply graduated pressure to the legs, which helps:
- Improve Blood Circulation: By enhancing venous return, compression socks prevent blood from pooling in the legs, reducing the risk of clot formation.
- Reduce Swelling: The pressure helps control swelling and edema, promoting faster healing.
- Support Muscle Recovery: By stabilizing the muscles, compression socks aid in reducing soreness and fatigue.
For those recovering from surgery, wearing compression socks can be a simple yet effective measure to mitigate the risk of serious complications and support the body’s healing process.
In conclusion, understanding the intricacies of post-surgery recovery and the potential complications is crucial for a successful healing journey. By being aware of risk factors, recognizing early signs, and implementing preventive measures such as compression socks, patients can navigate this recovery phase with confidence and care. Always consult with healthcare professionals to tailor a recovery plan that suits your specific needs and circumstances.
For Arthritis
Arthritis in Your Legs and Feet
Arthritis—the persistent, often debilitating inflammation of joints—affects millions of individuals globally. Its impact is widespread yet profoundly personal, touching the core of one’s daily life, particularly when it invades the legs and feet.
What is Arthritis?
Arthritis is not a single disease but a complex group of musculoskeletal disorders encompassing over 100 different conditions. The term “arthritis” itself translates to joint inflammation, which is the hallmark of the condition. In the legs and feet, arthritis can compromise mobility, causing pain, swelling, and even deformity.
How Common is It?
In the United Kingdom alone, arthritis affects approximately 10 million people. This statistic highlights a significant public health challenge, with osteoarthritis and rheumatoid arthritis being the most prevalent types.
Affected Areas
Arthritis in the legs and feet primarily targets joints like the knees, ankles, and smaller joints of the toes. These regions endure considerable stress from daily activities, making them prime candidates for arthritic changes.
Causes and Risk Factors
The causes of arthritis are multifaceted and vary with the type of arthritis.
- Age: As we age, the wear and tear on our joints increase, making osteoarthritis more likely.
- Genetics: A family history of arthritis can predispose individuals to the condition.
- Obesity: Excess weight places additional stress on weight-bearing joints, accelerating joint degeneration.
- Injuries: Previous joint injuries can lead to arthritis later in life.
- Occupation: Jobs involving repetitive stress on particular joints can contribute to arthritis.
- Gender: Women are more prone to rheumatoid arthritis, whereas men are more likely to develop gout.
Symptoms to Watch For
Recognizing the symptoms early can be crucial in managing arthritis effectively:
- Pain: A persistent ache in the affected joints, often worsening with activity.
- Swelling: Visible inflammation around the joints.
- Stiffness: Reduced range of motion, especially after periods of inactivity.
- Redness and Warmth: The affected area may appear reddened and feel warm to the touch.
- Deformity: In advanced stages, joints may lose their normal shape.
The Importance of Treatment
Ignoring arthritis can lead to severe complications, including chronic pain, significant joint damage, and disability. Early and proactive treatment is essential to slow progression, manage symptoms, and maintain quality of life.
Treatment Options
Arthritis treatment is multifaceted and aims to reduce symptoms and improve joint function:
- Medications: Pain relievers, anti-inflammatory drugs, and disease-modifying antirheumatic drugs (DMARDs) for rheumatoid arthritis.
- Physical Therapy: Exercises to strengthen muscles around joints and improve flexibility.
- Lifestyle Changes: Weight management and a balanced diet to reduce stress on joints.
- Surgical Interventions: In severe cases, joint repair or replacement may be necessary.
The Role of Compression Socks
Compression socks are a valuable tool in both the treatment and prevention of arthritis in the legs and feet. These specially designed socks apply graduated pressure to the legs, improving blood flow and reducing swelling.
How Compression Socks Help:
- Enhanced Circulation: By promoting better blood flow, compression socks help reduce the pooling of blood and fluids in the lower extremities, which can alleviate pain and swelling.
- Reduced Inflammation: Improved circulation can lead to less inflammation around the joints.
- Support and Stability: Compression socks provide additional support to the joints and surrounding muscles, which can help in managing pain and improving mobility.
- Prevention: Regular use of compression socks may help prevent the development of arthritis by maintaining leg health and reducing the strain on joints.
Conclusion
Arthritis in the legs and feet is a common yet challenging condition that requires a comprehensive approach to management. By understanding the causes, recognizing the symptoms, and exploring effective treatments, including the use of compression socks, individuals can take proactive steps to manage their arthritis and improve their quality of life. Remember, early intervention and consistent care are key to navigating the complexities of arthritis and ensuring a future with less pain and more mobility.
Compression socks can help improve blood circulation, reduce swelling, and provide support to the legs, making them useful in these various conditions and situations. Always consult with a healthcare professional before using compression socks, especially if you have underlying health conditions.
Why Choose Footreviver Compression Socks?
Now that we’ve discussed the benefits of compression therapy and the situations where these socks can be most helpful, let’s delve into the specific features that make Footreviver Compression Socks stand out as the perfect choice for you.
Key Features:
- Graduated Compression: Footreviver Compression Socks incorporate graduated compression technology, which means the pressure is highest at the ankle and decreases as it moves up the leg. This design ensures optimal blood flow and maximum comfort. Graduated compression not only helps in reducing swelling and fatigue but also enhances athletic performance and speeds up recovery by ensuring efficient circulation.
- Comprehensive Support: Footreviver Compression Socks are designed to support various parts of your lower legs and feet, including the arches, heels, achilles tendons, calves, and shins. This all-encompassing support helps reduce strain and pressure on these areas, which can prevent the development or worsening of conditions like plantar fasciitis, Achilles tendinitis, and shin splints. The comprehensive support also aids in recovery from strenuous activities and injuries.
- Shock Absorption: These socks are equipped with cushioning in strategic areas to absorb impact and reduce stress on your feet and lower legs. This shock absorption is particularly beneficial for runners, hikers, and individuals engaged in high-impact activities, as it can help prevent injuries such as stress fractures and joint pain. The cushioning also adds an extra layer of comfort, making long periods of wear more bearable.
- High-Quality Materials: Crafted from a blend of breathable, moisture-wicking fabrics, these socks keep your feet dry and comfortable throughout the day. The materials are also durable, ensuring long-lasting use. The anti-bacterial properties of the fabric help in preventing odor and infections, making them ideal for extended wear.
- Ergonomic Design: Thoughtfully designed to fit the contours of your feet and legs, these socks provide a snug yet comfortable fit without slipping or bunching. The reinforced heel and toe areas add extra durability and comfort. The seamless construction helps in avoiding blisters and chafing, making them perfect for both athletic and everyday activities.
- Versatility: Suitable for a wide range of activities, from athletic performance to everyday wear, Footreviver Compression Socks are versatile enough to meet the needs of various users. Whether you’re running a marathon or recovering from surgery, these socks offer the support you need. They are also beneficial for long-duration travel, preventing deep vein thrombosis (DVT) and leg swelling.
- Copper-Infused Fibers: Footreviver Compression Socks are infused with copper fibers, known for their antibacterial properties. Copper helps to kill bacteria and fungi, reducing odor and keeping your feet fresh and healthy. Additionally, copper is believed to promote better skin health and enhance circulation.
- Advanced Moisture Control: Footreviver Compression Socks feature advanced moisture-wicking technology that actively draws sweat away from your skin, keeping your feet dry and comfortable. This feature helps to prevent the growth of odor-causing bacteria and fungal infections, making the socks ideal for prolonged use in various conditions.
- Seamless Toe Construction: Footreviver Compression Socks feature a seamless toe design to minimize irritation and friction. This construction method eliminates uncomfortable seams that can cause blisters and pressure points, ensuring a smooth and comfortable experience, especially for sensitive skin.
- Temperature Regulation: These socks are engineered with advanced temperature-regulating materials that adapt to your body’s needs. They keep your feet warm in colder conditions and cool in warmer environments, providing year-round comfort and making them suitable for any climate or season.
- Easy Maintenance: Footreviver Compression Socks are easy to care for, featuring machine-washable fabric that retains its elasticity and form even after multiple washes. This makes them a convenient and practical choice for everyday use.
In sum, Footreviver Compression Socks are an excellent investment in your health and wellbeing. By choosing these socks, you’re opting for a product that is not only backed by scientific principles but also designed with your comfort and daily needs in mind. If you’re seeking a practical, effective solution to enhance your circulation, reduce discomfort, and support your overall leg health, look no further than Footreviver Compression Socks.
Would you like more detailed information about any specific feature, or do you have any other questions? Feel free to ask—we’re here to help!
Disclaimer:
The information provided here is for guidance purposes only and should not be substituted for actual medical advice. It’s crucial to avoid self-diagnosis and ensure proper diagnosis by consulting a medical professional. If you are experiencing any issues with your feet or legs, especially if you have an underlying health condition, it’s important to consult a doctor right away. This is because conditions like poor circulation, diabetic foot, Deep Vein Thrombosis (DVT), and others require precise diagnosis and tailored treatment plans.
A doctor will be able to provide you with the best advice and treatment recommendations for your specific health needs, including whether wearing compression socks is right for you. Here at NuovaHealth, we ensure that all the products we sell are expertly designed and made using medical-grade materials. Our products are tested to ensure their efficacy. However, compression socks may not be suitable for everyone.
In some cases, wearing compression socks can exacerbate certain conditions. For example, individuals with severe peripheral arterial disease may find compression socks worsen their condition. Similarly, those with skin infections or open wounds on their legs should avoid using compression socks until these issues are resolved. Always seek professional medical advice to determine the best course of action for your health.
At NuovaHealth, we are committed to your well-being. Please remember that medical advice from your healthcare provider is indispensable in ensuring the best possible outcomes for your health.
Average Rating
5.00
Rated 5.00 out of 5 based on 3 customer ratings
035 Star
100%
4 Star
0%
3 Star
0%
2 Star
0%
1 Star
0%
Add a review Cancel reply
3 Reviews For This Product
Fast & Secure Checkout Through Paypal
Pay with Paypal the secure payment gateway that accepts all credit and debit cards. Paypal is free and secure and no credit or bank information is ever stored or shared with us.
Fast Dispatch
Enjoy your items soon with quick dispatch via Royal Mail First Class. Expect to have your items between 1-3 days for domestic orders. 7-10 Working days for international orders.
Return Policy – 30 Day Money Back Guarantee
We are so confident that you will just love our product that we offer a full 30 day money back guarantee. In the unlikely event, you are unhappy with your purchase you can simply return it within 30 days for a refund. Please contact us via the form on the contact us page to start your return.
To return an item please send it to: Nuova Health UK, 81 Highfield Lane, Waverley, Rotherham, S60 8AL. Please include a note with your order id so we know who to refund. Please retain your postage receipt as proof of postage. All that we ask is that the item is in the original packaging and unused.



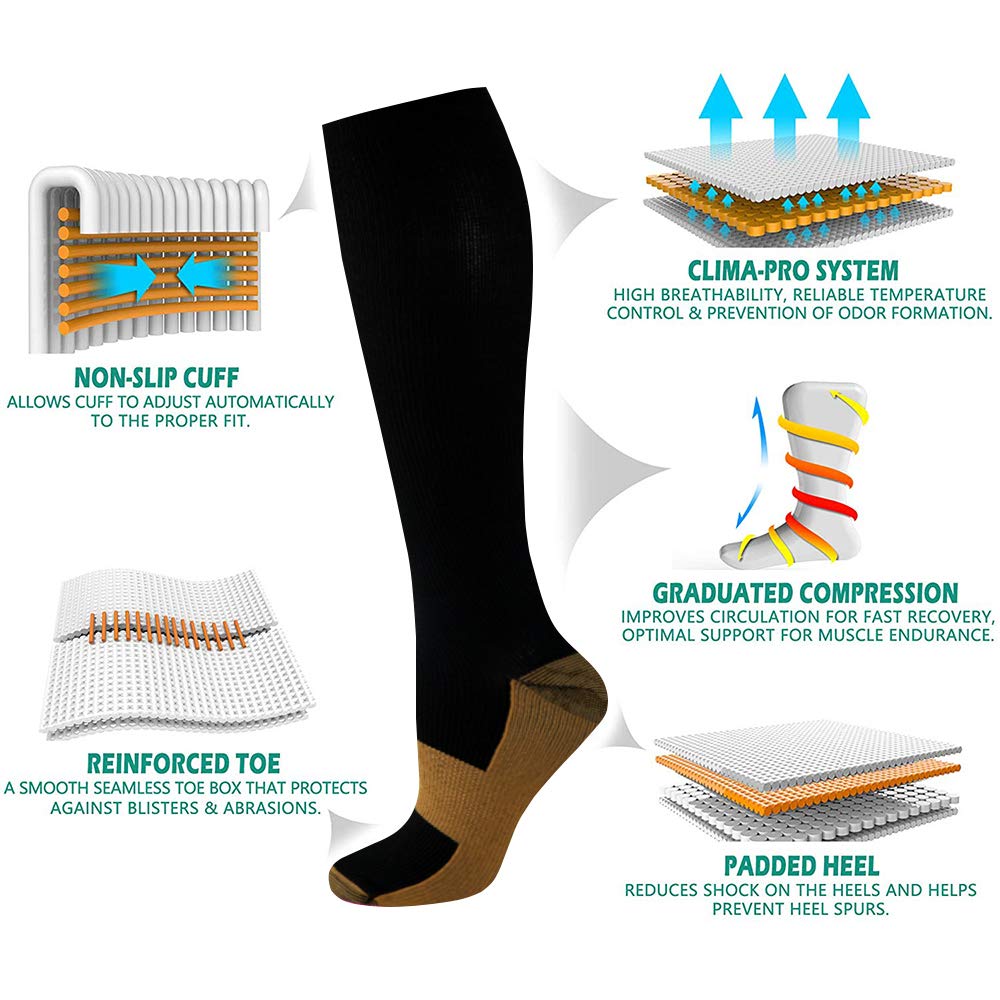

by Annette
Bought these for my 77 year old dad and he said that they are a very good support sock.
by John Marlow
Purchased these before and great quality product
by Ian Alexander
Bought these FootReviver socks two months ago and boy, oh boy, they’ve been a game-changer! As an arthritis sufferer, my feet used to throb at the end of a long day. These socks, they’ve made such a difference. Quality? Top drawer. Not only do they support and stabilize my feet, but they make me feel like I’m walking on clouds. Highly recommend these, folks!